JACC:左心耳封闭 vs口服抗凝,治疗房颤效果相当出血少!
2022-01-07 MedSci原创 MedSci原创
心房颤动(AF)是栓塞性脑卒中和其他血栓栓塞性并发症的常见原因。
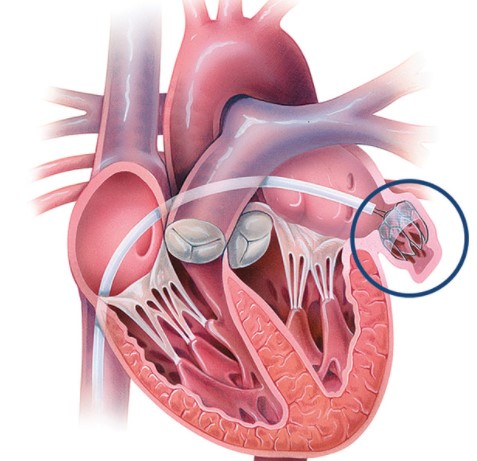
心房颤动(AF)是栓塞性脑卒中和其他血栓栓塞性并发症的常见原因。AF患者的血栓栓塞主要来源于左心耳(LAA)。一项研究回顾了多项通过经食管超声心动图、心脏手术或尸检评估左心房血栓位置的研究,发现在无风湿性心脏病的AF患者中,90%的左心房血栓位于LAA。
LAA是AF患者血栓栓塞的重要来源,据此可行LAA结扎、切除或封堵术,尤其是对于具有抗凝指征但不能接受长期口服抗凝治疗(DOAC)的患者。PRAGUE-17(左心耳封闭术与房颤新型抗凝剂)试验表明,左心耳封闭术(LAAC)在预防高危房颤(AF)患者的重大神经、心血管或出血事件方面不逊于直接口服抗凝剂。
为了评估PRAGUE-17试验中预设的长期(4年)随访结果,捷克布拉格查尔斯大学第三医学院心脏中心和克拉罗夫斯克维诺拉迪大学医院近期对该试验数据进行进一步的分析,结果发表在JACC杂志上。

PRAGUE-17是一项随机非劣效试验,对非瓣膜性房颤、有心肌栓塞史、临床相关出血或CHA2DS2-VASc≥3和HASBLED≥2的患者进行经皮LAAC(Watchman或Amulet)与DOACs(95%阿哌沙班)的对比。主要终点是心脑血管栓塞事件(中风、短暂性脑缺血发作或全身性栓塞)、心血管死亡、临床相关出血或手术/设备相关并发症(仅LAAC组)的综合。主要分析是修改后的意向治疗。
结果显示,该研究随机调查了402名房颤患者(每组201人,年龄73.3±7.0岁,65.7%为男性,CHA2DS2-VASc 4.7±1.5,HASBLED 3.1±0.9)。经过3.5年的中位随访(1354患者年),根据修改后的意向性治疗,LAAC在主要终点方面不逊于DOACs(亚分布HR=0.81;95%CI:0.56-1.18;P=0.27;非劣效性P=0.006)。
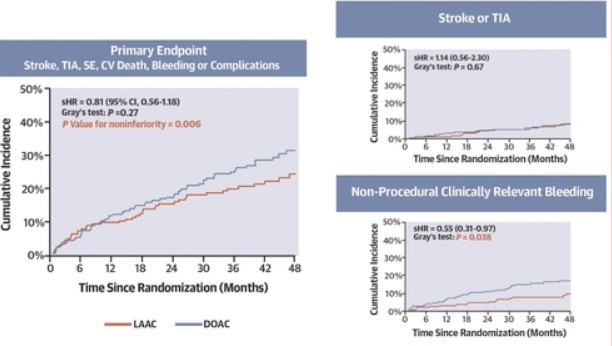
对于复合终点的组成部分,相应的sHRs为:心血管死亡=0.68(95%CI:0.39-1.20),所有中风/短暂性脑缺血发作=1.14(95%CI:0.56-2.30),临床相关出血=0.75(95% CI:0.44-1.27),非程序性临床相关出血=0.55(95% CI:0.31-0.97)。此外,主要终点结果在按方案分析(sHR=0.80;95%CI:0.54-1.18)和治疗中分析(sHR=0.82;95%CI:0.56-1.20)中相似。
综上,在PRAGUE-17的长期随访中,LAAC在预防主要心血管、神经系统或出血事件方面仍不逊于DOACs。此外,使用LAAC后,非手术性出血明显减少。
参考文献:
4-Year Outcomes After Left Atrial Appendage Closure Versus Nonwarfarin Oral Anticoagulation for Atrial Fibrillation. J Am Coll Cardiol. 2022 Jan, 79 (1) 1–14
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#JACC#
28
学习了!
51
#ACC#
34
#左心耳#
44