Ther Adv Med Oncol:洛铂新辅助治疗可改善三阴性乳腺癌患者预后
2022-07-04 MedSci原创 MedSci原创
洛铂新辅助治疗可提高三阴性乳腺癌的总病理完全缓解率和总缓解率
三阴性乳腺癌 (TNBC) 是一种侵袭性乳腺癌亚型,占所有乳腺癌的 12%-17%,缺乏雌激素受体 (ER)、孕激素受体 (PR) 和人表皮生长因子受体 2 (HER2)。由于缺乏靶向治疗,与其他乳腺癌亚型相比,TNBC 具有更大的转移潜力、更高的复发率、更差的临床结果和更低的生存率。
本文汇报了一项评估以洛铂为基础的新辅助化疗联合辅助治疗TNBC的随机、开放标签的II期试验的5年随访结果。
该研究招募了年满18岁的未治疗过的、可手术的I-III期TNBC患者,随机分成两组,一组(TE组,n=99)予以4个疗程的多西紫杉醇(T,75mg/m2)+表柔比星(E,80mg/m2)治疗,3周为一疗程;另一组(TEL组,n=101)予以相同治疗方案的基础上加用洛铂(L,30mg/m2)。两组术后均再予以两个疗程治疗。主要终点包括总病理完全缓解率(tpCR)和总缓解率(ORR),次要终点包括无病生存率、总生存率和长期安全性。
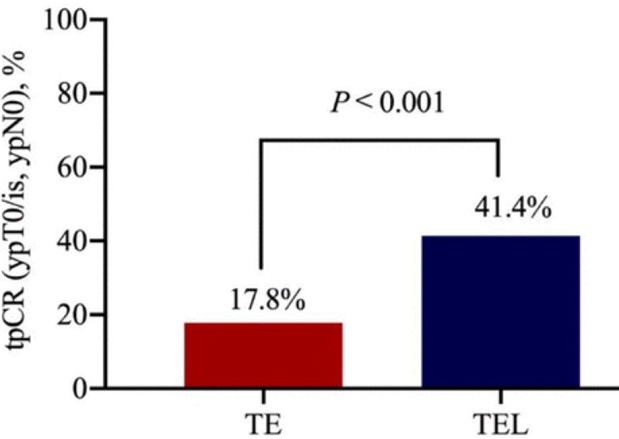
两组的病理缓解率
中位随访了48.2个月。TEL组和TE组的tpCR分别是41.4%和17.8%(p<0.001)。TEL组和TE组的DFS比较的风险比(HR)为0.44(p=0.028)。加用洛铂导致两组的总生存率差异的HR为0.44(p=0.061)。TEL组和TE组的总缓解率分别是92.9%和74.3%(p=0.001)。TEL组患者更容易出现III-IV级贫血和血小板减少症。未观察到洛铂相关死亡或长期毒性风险增加。
两组的DFS和OS
总之,洛铂新辅助治疗可提高三阴性乳腺癌的总病理完全缓解率和总缓解率,副作用可耐受,且有改善长期生存率的趋势。
原始出处:
Yan Wenting,Wu Xiujuan,Wang Shushu et al. Lobaplatin-based neoadjuvant chemotherapy for triple-negative breast cancer: a 5-year follow-up of a randomized, open-label, phase II trial.[J] .Ther Adv Med Oncol, 2022, 14: 17588359221107111.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#铂#
54
#患者预后#
51
#Oncol#
46
#阴性乳腺癌#
0
#新辅助#
43
#三阴性#
54
#乳腺癌患者#
45
#Med#
33