ATVB:高密度脂蛋白与主动脉瓣钙化长期发生率和进展的关系
2022-08-26 MedSci原创 MedSci原创
在多民族人群中,HDL-C、HDL-P、大HDL-P和缺乏apoc3的HDL-C与AVC的长期发生率和进展呈负相关。
主动脉瓣钙化(AVC)与动脉粥样硬化具有相同的病理特征。主动脉瓣组织中检测到脂蛋白成分,包括HDL(高密度脂蛋白)。HDL测量与心血管疾病呈负相关,但与AVC长期进展的关系尚不清楚。
近日,心血管领域权威杂志Arteriosclerosis, Thrombosis, and Vascular Biology上发表了一篇研究文章,在这项研究中,研究人员探究了HDL胆固醇、颗粒、apoc3定义的HDL亚型,以及CETP(胆固醇酯转移蛋白)的含量和活性与AVC长期发病率和进展之间的关系。
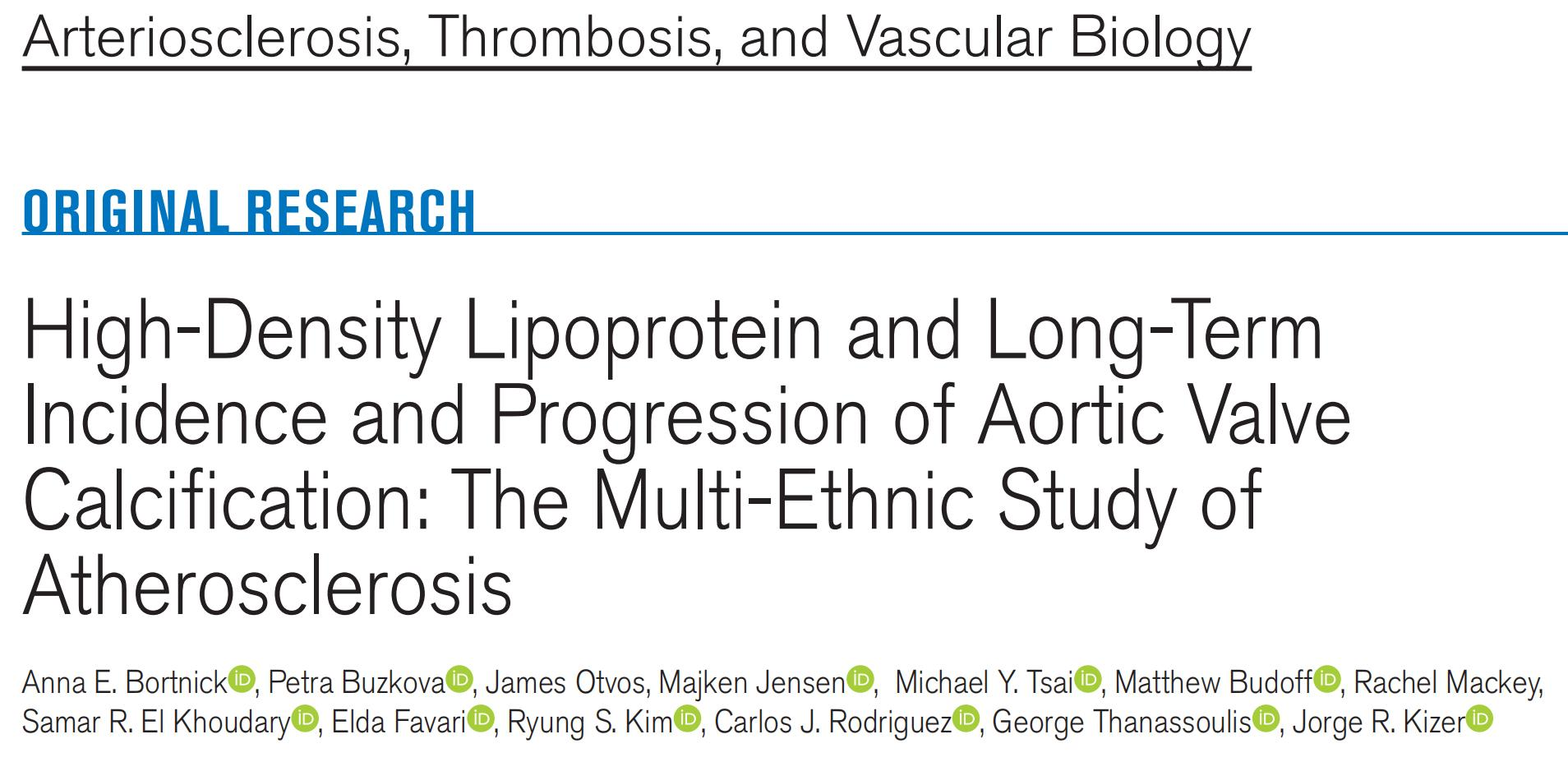
研究人员使用线性混合效应模型来评估基线HDL指数与AVC之间的相关性。在多民族动脉粥样硬化研究(n=6814)中位随访时间为8.9年(最长11.2年),通过3次连续计算机断层扫描Agatston评分来量化AVC。
经过调整后,较高浓度的HDL-c(高密度脂蛋白胆固醇)、HDL-p(HDL颗粒)、大HDL-p和缺乏apoc3的HDL-c与AVC的发生率/进展显著相关,较高的CETP含量也与AVC的发生率/进展显著相关。在主要分析中,小型或中型HDL-P、包含apoc3的HDL-C或CETP活性与AVC的发生率/进展均不显著相关。当合并在一起时,只观察到HDL-C与其的显著关联,而HDL-P与其无显著关联。在探索性分析中,HDL-c、HDL-p、大HDL-p和apocc3缺失HDL与AVC发生率/进展的负相关在≥65岁的成年人、男性和白人参与者中更明显。在这些亚组中,仅有包含apoc3的HDL-C与AVC呈正相关。
在多民族人群中,HDL-C、HDL-P、大HDL-P和缺乏apoc3的HDL-C与AVC的长期发生率和进展呈负相关。对高密度脂蛋白组成和机制的进一步研究可能有助于理解减缓AVC的机制。
原始出处:
Anna E. Bortnick.et al.High-Density Lipoprotein and Long-Term Incidence and Progression of Aortic Valve Calcification: The Multi-Ethnic Study of Atherosclerosis.ATVB.2022.https://www.ahajournals.org/doi/10.1161/ATVBAHA.122.318004
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#TVB#
52
#发生率#
55
#主动脉瓣#
51
#主动脉#
58
#脂蛋白#
83
#主动脉瓣钙化#
53