Science揭秘:这种胆固醇,让肝脏疾病有救了!
2021-08-13 zyyzjy MedSci原创
最新发表在《Science》杂志上一篇研究显示小肠分泌的HDL3可通过阻断肠道细菌产生的炎症反应来发挥肝脏保护作用。
高密度脂蛋白(HDL)胆固醇是公认的“好胆固醇”,既往的大量研究显示其可降低心血管疾病的风险。尽管近些年几种升高HDL-C的药物实验结果并没有显示硬终点获益,其“好胆固醇”的称号遭受了一些质疑和挑战,但仍陆续有研究结果为其正名。 最新发表在《Science》杂志上一篇研究显示小肠分泌的HDL3可通过阻断肠道细菌产生的炎症反应来发挥肝脏保护作用。 此项研究中圣路易斯的华盛顿大学医学院的研究者通过荧光标记小鼠肠源性HDL3,发现HDL3主要由回肠分泌,分泌后并不像其他乳糜微粒那样进入淋巴管,而是迅速进入门静脉,与其内的脂多糖结合蛋白(LBP)结合,阻止肠道损伤引起的革兰氏阴性细菌分泌的脂多糖激活枯否细胞,从而抑制炎症反应,保护肝脏免受炎症及纤维化的损伤。 Enterically derived high-density lipoprotein restrains liver injury through the portal vein. Science 373, 410 (2021) 23.doi.org/10.1126/science.abe6729 研究者尝试将小鼠部分小肠切除(50%或75%的小肠,保留小肠近端部分和回肠末端),结果显示门静脉内LPS生物活性升高,肝损伤加重。原因可能与更短的肠道使HDL3产生减少,同时手术本身会导致肠道的损伤产生更多的脂多糖有关。 此外研究者给予小鼠口服低剂量GW3965(一种LXRs激动剂,LXRs是控制HDL相关基因表达的转录因子),结果显示其可保护肝脏免受炎症和纤维化影响,此作用取决于其增加肠道HDL分泌的能力。 而在人体中,儿科专家发现一些早产儿因坏死性小肠结肠炎行手术切除一部分肠道后经常会患上肝病,动物实验的结果也许能给予一部分解释。 基于上述实验发现,HDL有望成为今后肝损伤治疗的一个新的方向。 health.harvard 除了心血管、肝脏的保护作用外,研究显示HDL对肾脏、脑、肺脏、内分泌系统同样发挥保护作用。 肾 同样,在慢性肾病和终末期肾病患者中HDL-c水平也会显著降低并出现功能障碍,失去其抗氧化应激、抗炎、保护内皮功能等功能,从而加速患者肾脏疾病的进展。 HDL abnormalities in nephrotic syndrome and chronic kidney disease. Nat Rev Nephrol 2016,12(1):37-47. doi:10.1038/nrneph.2015.180.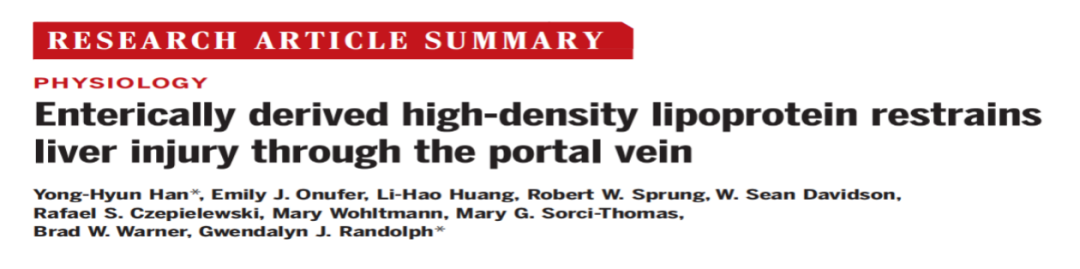
脑
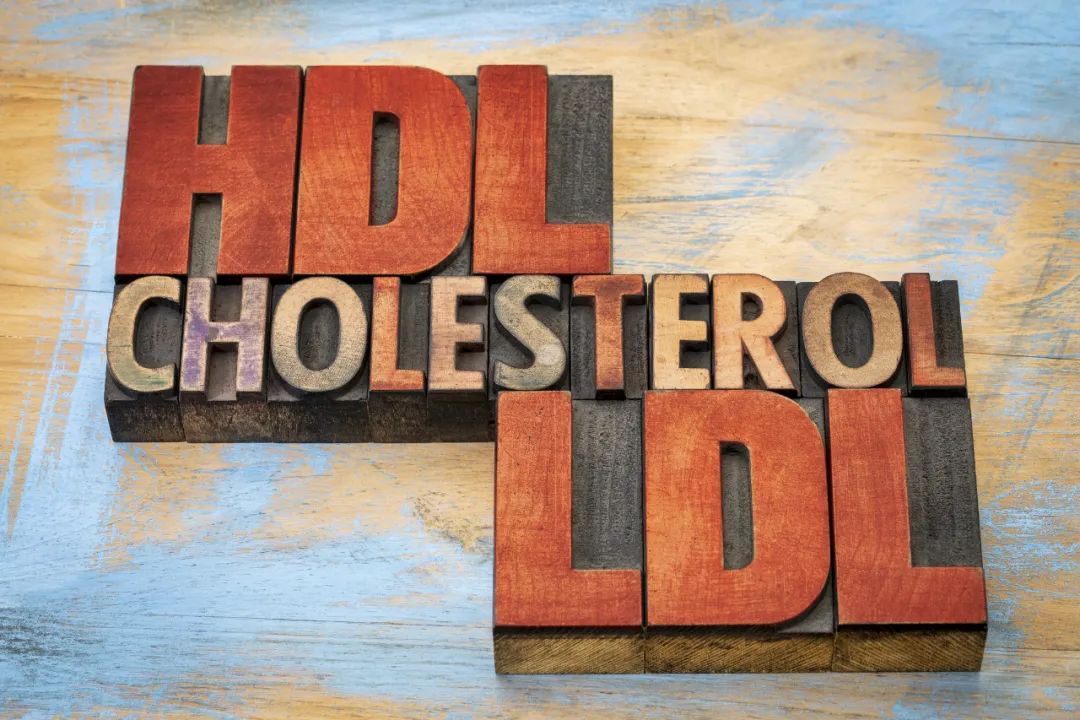
胆固醇是哺乳动物的外周和中枢神经系统的重要组成部分。中枢神经系统中HDL的主要载脂蛋白成分是载脂蛋白E,由星形胶质细胞和小胶质细胞产生。低HDL-C水平与认知障碍和各种神经退行性疾病有关。
HDL的抗氧化和抗炎特性可影响大脑中的炎症反应。HDL介导的胆固醇反向转运可降低脑血管的动脉粥样硬化负担,从而抑制血管性痴呆的进展。HDL对内皮功能的保护作用可影响脑血管功能,影响神经元活动,从而发挥脑保护作用,减少多种神经系统疾病的发生发展。
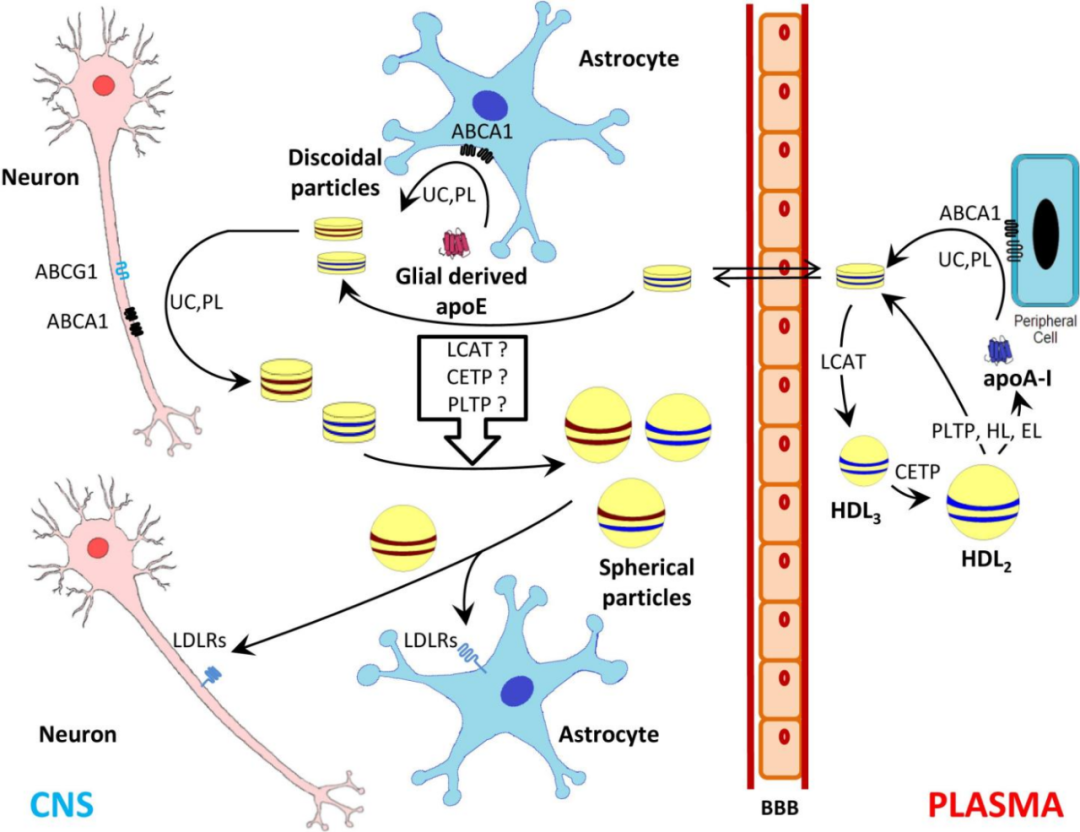
HDL AND CHOLESTEROL HANDLING IN THE BRAIN. Cardiovasc Res 2014, 103(3):405-13.
代谢
HDL及其主要载脂蛋白A-I (ApoA-I)现已被证实通过多种机制影响糖代谢。临床研究发现T2DM患者中,无论是通过短期重组HDL输注引起的急性HDL升高,还是通过胆固醇酯转移蛋白(CETP)抑制剂引起的慢性HDL升高,都能降低血糖。HDL可能通过不同的机制在多个器官(如胰腺、骨骼肌、心脏、脂肪、肝脏、大脑)的作用下介导对葡萄糖代谢的影响:(i)胰腺β细胞分泌胰岛素(ii)胰岛素非依赖性葡萄糖摄取(iii)胰岛素敏感性。

HDL and glucose metabolism: current evidence and therapeutic potential. Front Pharmacol, 2015,6:258. doi: 10.3389/fphar.2015.00258.
肺
人体检测显示脓毒症所致ARDS患者血浆中HDL-C和HDL-载脂蛋白(apoA-I、apoA-II、apoA-IV、pak - iii)水平较健康对照者明显降低,且HDL组分也发生了显著变化。体内研究表明,ARDS大鼠的HDL加重了脓毒症所致的ALI,提示HDL在脓毒症性ARDS过程中发生了不良功能转变。而这些有害作用与肺内皮功能障碍有关,而肺与LPS增加有关。这些研究结果揭示了HDL成分的重塑使内皮功能障碍导致脓毒症性ARDS的发生,也证明了循环HDL在调节肺泡内稳态中的重要性。
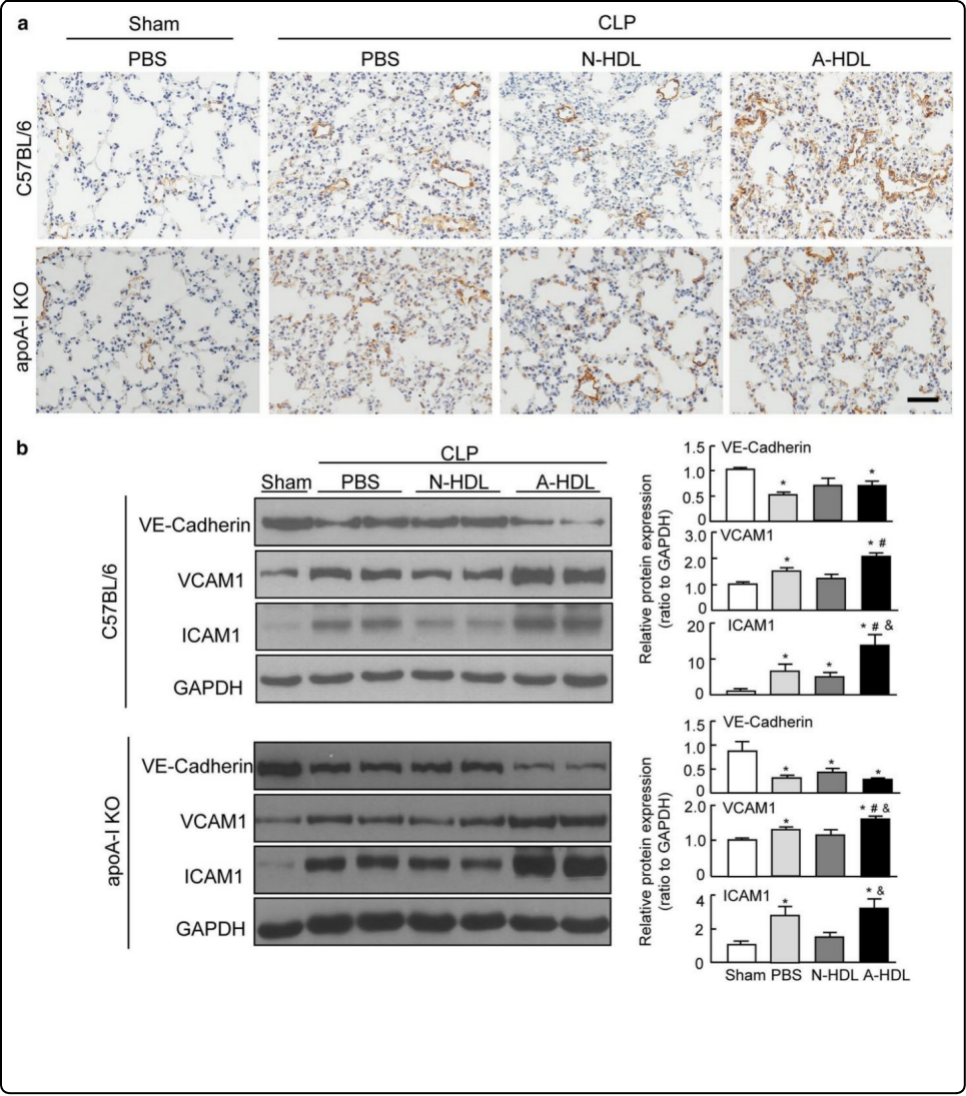
The HDL from septic-ARDS patients with composition changes exacerbates pulmonary endothelial dysfunction and acute lung injury induced by cecal ligation and puncture (CLP) in mice.. Respir Res (2020) 21:293 .doi.org/10.1186/s12931-020-01553-3.
肿瘤
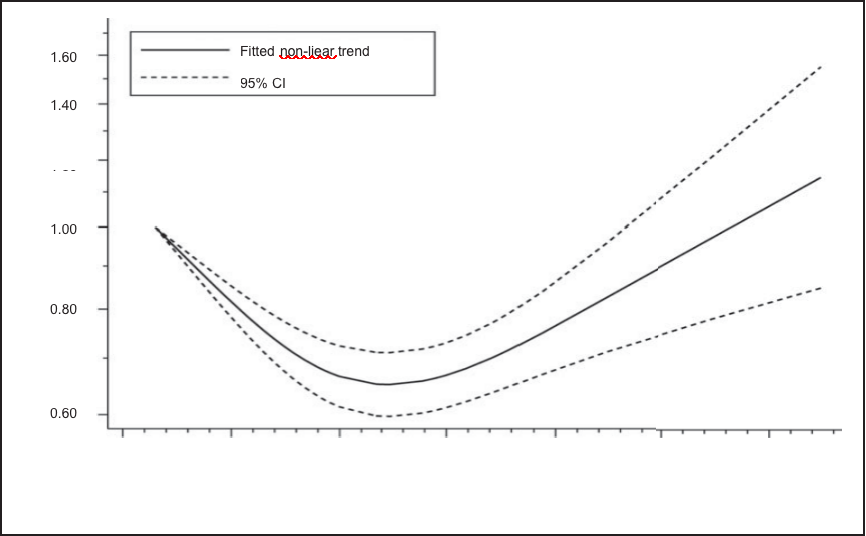
除脏器保护作用之外,一些观察性研究显示HDL-C水平降低与多种癌症相关包括结直肠癌、肺癌、乳腺癌、卵巢癌、甲状腺癌、胃癌等。高HDL-水平与大多数肿瘤类型的OS和DFS呈正相关,与死亡率呈负相关。一些研究甚至表明,HDL-C可以作为某些癌症患者的预后标志物。
一项涉及145万参与者的荟萃分析显示HDL-C和癌症风险之间呈J形关联,当HDL-C水平为64-68 mg/dL时,癌症风险最低。
此结果表明两者并非呈线性关系,可能存在多种影响因素,年龄、性别、疾病阶段、肿瘤类型和许多其他因素(如癌症治疗方式、氧化应激等)等,需进一步的研究确定。
HDL and cancer - causality still needs to be confirmed? Update 2020.Semin Cancer Biol 2021, 73:169-177. doi.org/10.1016/j.semcancer.2020.10.007.
HDL对多个脏器、多种疾病均有保护作用,未来我们可能会发现更多它的好。
参考文献:
1.Enterically derived high-density lipoprotein restrains liver injury through the portal vein. Science 373, 410 (2021) 23.doi.org/10.1126/science.abe6729
2.HDL abnormalities in nephrotic syndrome and chronic kidney disease. Nat Rev Nephrol 2016,12(1):37-47. doi:10.1038/nrneph.2015.180.
3.HDL and cholesterol handling in the brain. Cardiovascular Research, 2014,103(3), 405–413. doi:10.1093/cvr/cvu148
4.HDL and glucose metabolism: current evidence and therapeutic potential. Front Pharmacol, 2015,6:258. doi: 10.3389/fphar.2015.00258.
5.The HDL from septic-ARDS patients with composition changes exacerbates pulmonary endothelial dysfunction and acute lung injury induced by cecal ligation and puncture (CLP) in mice.. Respir Res (2020) 21:293 .doi.org/10.1186/s12931-020-01553-3.
6.HDL and cancer - causality still needs to be confirmed? Update 2020.Semin Cancer Biol 2021, 73:169-177. doi.org/10.1016/j.semcancer.2020.10.007.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#肝脏疾病#
49
#SCIE#
29
已读已读已读已读已读已读,学学习学习学习学习学习学习。受益匪浅
48
学习了,怎么提高
56
学习了!
60
学习!
56