血脑屏障(BBB)在很大程度上限制了潜在的治疗分子进入大脑的机会。近年来,聚焦超声(FUS)和静脉注射微泡的组合已被证明可以在特定的大脑目标处短暂地破坏BBB。
图1: 论文封面图
在阿尔茨海默病(AD)、肌萎缩侧索硬化症和帕金森病(PD)患者中,已经开展了一些试点临床试验,分别在前额白质、海马体、初级运动皮层和顶枕部连接处进行BBB开放。这些报告证明了这种方法的可行性和安全性,包括在这些常见的神经退行性疾病中重复FUS介导的BBB开放达三次。
帕金森病的特点是进行性的纹状体(尾状核)多巴胺能神经支配,与运动性发病的基本特征有关。因此,黑质体投射可以说是在帕金森病早期提供神经恢复性疗法的主要目标。然而,众所周知,纹状体对各种代谢紊乱和物理损伤相当脆弱。因此,在PD中定义BBB纹状体开放本身的安全性和影响是迈向该方法可能的治疗应用的第一步。
相反,虽然BBB的开放主要是为了促进大脑接触假定的治疗方法,但它与实验和AD患者8的淀粉样细胞外沉积的减少有关。在小鼠中,这种针对AD病理学的效果似乎通过同时提供针对β-淀粉样蛋白和tau的抗体而得到加强。
有趣的是,路易体病理和AD病理在PD与痴呆(PDD)中都很突出,而且,PDD患者的纹状体β-淀粉样蛋白积累比没有痴呆的患者更常见。
藉此,马德里Fundacion Hospitales de Madrid的José A. Pineda-Pardo等人,假设:纹状体BBB开放是可行的、可逆的、安全的和良好的容忍性。另外,关于安全性,他们测试了反复暴露和双侧干预是否与多巴胺能的进一步丧失有关。最后,研究纹状体BBB开放是否会减少纹状体β-淀粉样蛋白的负担,正如在大脑皮层和海马区所描述的那样。
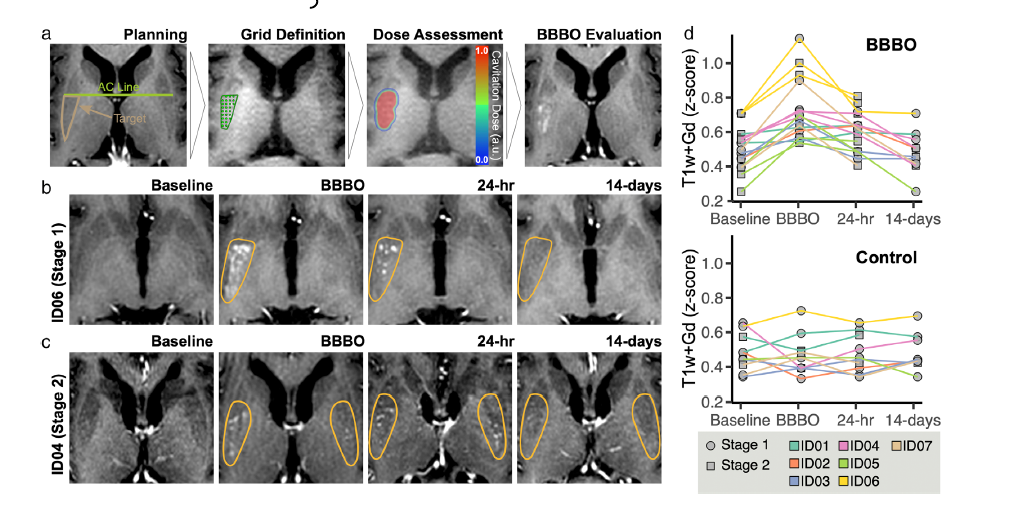
图2:论文结果图
共有7名患有认知障碍的PD患者接受了后壳核BBB开放治疗。分两个疗程进行,间隔时间为2至4周,其中第二个疗程包括3名患者的双侧斗室开放。
主要结果测量包括局灶性纹状体BBB开放的安全性和可行性。运动和认知功能、磁共振成像(MRI)、18F-氟多巴(FDOPA)和β-淀粉样蛋白PET(正电子发射断层成像)图像的变化被确定。
他们发现:该手术是可行的,耐受性良好,没有严重的不良事件。在随访中没有发现运动和认知(神经心理学测试)功能方面的神经相关变化。
MRI显示,治疗后不久(24小时至14天),壳核BBB关闭,排除了出血性和缺血性病变。目标区域的β-淀粉样蛋白摄取量有不连续但明显的减少,FDOPA PET没有变化。这些初步结果表明,FUS介导的纹状体BBB开放是可行和安全的,因此可以成为一种有效的工具,以促进PD中推定的神经恢复性分子的传递。
原文出处:
Pineda‐Pardo JA, Gasca‐Salas C, Fernández‐Rodríguez B, et al. Striatal Blood–Brain Barrier Opening in Parkinson’s Disease Dementia: A Pilot Exploratory Study. _Movement Disorders_. Published online June 28, 2022:mds.29134. doi:[10.1002/mds.29134](https://doi.org/10.1002/mds.29134)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#disorder#
63
#预防帕金森#
54
#Dis#
47
#ERS#
41
#Disord#
44
#disorders#
37
#血脑屏障#
52
#期刊论坛##学习#
58
不错的文章
39
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
43