Radiology:基于乳腺钼靶的放射组学特征在导管原位癌上分期的预测价值
2022-03-10 MedSci原创 MedSci原创
乳腺导管原位癌(DCIS)是分期为0期的乳腺癌,约占所有新诊断乳腺癌的14.9%。虽然DCIS没有生命危险,许多DCIS病例可能永远不会发展为浸润性癌症,但它是浸润性导管癌进展的潜在发现。
 乳腺导管原位癌(DCIS)是分期为0期的乳腺癌,约占所有新诊断乳腺癌的14.9%。虽然DCIS没有生命危险,许多DCIS病例可能永远不会发展为浸润性癌症,但它是浸润性导管癌进展的潜在发现。在活检证实为DCIS的患者中,有0%-26%的患者在最终手术时发现有并发的浸润性导管癌。目前,手术切除是治疗DCIS的标准治疗手段。然而,人们仍存在对DCIS过度治疗的担忧。
乳腺导管原位癌(DCIS)是分期为0期的乳腺癌,约占所有新诊断乳腺癌的14.9%。虽然DCIS没有生命危险,许多DCIS病例可能永远不会发展为浸润性癌症,但它是浸润性导管癌进展的潜在发现。在活检证实为DCIS的患者中,有0%-26%的患者在最终手术时发现有并发的浸润性导管癌。目前,手术切除是治疗DCIS的标准治疗手段。然而,人们仍存在对DCIS过度治疗的担忧。
先前的研究已经探讨了经活检证实的DCIS患者中存在浸润性癌症有关的因素,包括肿块、结构变形、不对称性、病变可触及性和病变大小在内的乳腺钼靶表现,但表现为纯钙化的DCIS也有潜伏着侵袭性病变的可能。对放射科医生来说,预测仅表现为钙化的DCIS患者的分期一直是个难题。
近日,发表在Radiology杂志的一项研究评估了通过乳腺放射学特征预测根据活检结果被诊断为DCIS的患者隐匿性浸润癌存在方面的表现和临床价值,为提高患者的生存期并减少不必要的治疗提供有价值的参考依据。
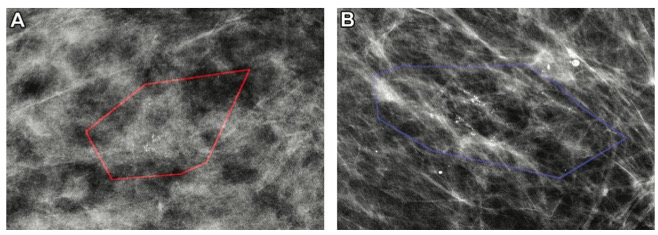
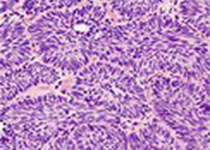
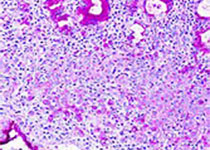
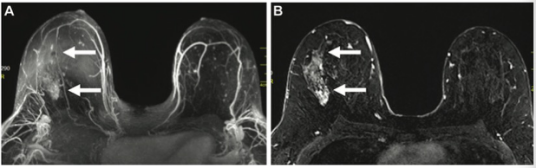
图 经活检证实的原位导管癌(DCIS)患者的乳腺钼靶图像。(A)55岁女性,仅被诊断为DCIS;模型正确分类为阴性发现。(B) 64岁女性,活检为DCIS,但随后上升为浸润性乳腺癌;模型正确分类为阳性发现。红色和蓝色的多边形显示了由放射科医生标注的病变。
本研究发现,从乳腺钼靶中得到的放射学特征可以对导管原位癌(DCIS)的隐性浸润性乳腺癌进行分类,其性能优于仅使用单独的临床标准。这表明,使用成像算法来改善病人护理及诊治成为可能,并可协助临床选择病人进行临床试验。
原文出处:
Rui Hou,Lars J Grimm,Maciej A Mazurowski,et al.Prediction of Upstaging in Ductal Carcinoma in Situ Based on Mammographic Radiomic Features.DOI:10.1148/radiol.210407
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#原位癌#
39
学习
45
学习学习学习学习学习学习学习学习学习学习学习学习学习学习
45
#预测价值#
35
学习
57
#学习#
55
乳腺#钼靶#的#放射组学#特征在#导管原位癌#
108