Am J Med Sci:慢性完全闭塞性经皮冠状动脉介入治疗老年患者的临床疗效
2018-07-10 MedSci MedSci原创
目前尚未有研究探究冠状动脉慢性完全闭塞(CTO)经皮冠状动脉介入治疗(PCI)对老年CTO患者预后的影响。近日,安贞医院的一项研究对此进行了探究。研究纳入了2011年1月至2013年12月期间的445名CTO-PCI患者,根据年龄分为老年组(≥75岁,n=120,27.0%)和非老年组(<75岁,n=325,73.0%),随访3年,观察两组患者的术中与长期预后情况。主要研究终点为3年随访时心绞痛住
目前尚未有研究探究冠状动脉慢性完全闭塞(CTO)经皮冠状动脉介入治疗(PCI)对老年CTO患者预后的影响。近日,安贞医院的一项研究对此进行了探究。
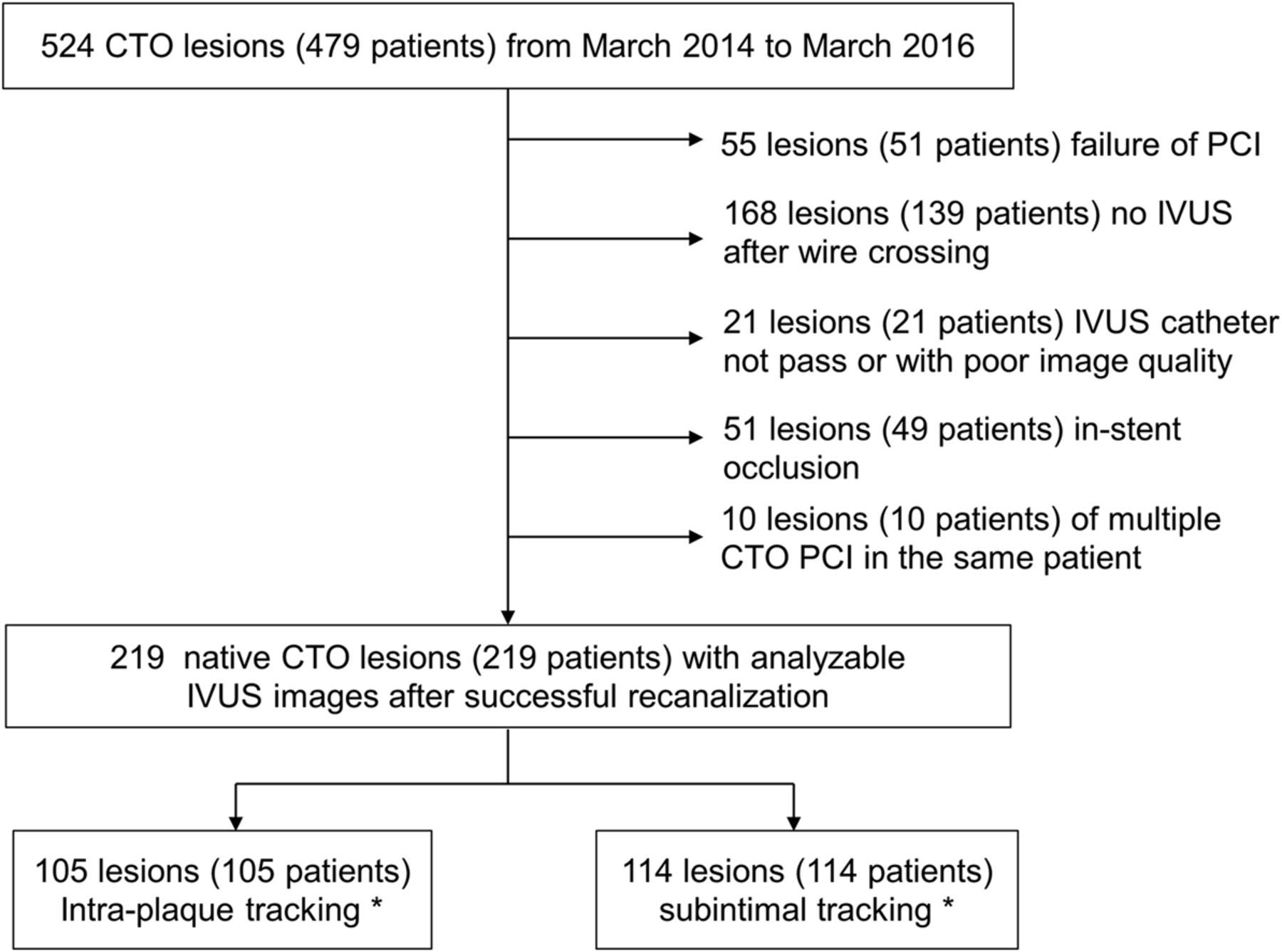
研究纳入了2011年1月至2013年12月期间的445名CTO-PCI患者,根据年龄分为老年组(≥75岁,n=120,27.0%)和非老年组(<75岁,n=325,73.0%),随访3年,观察两组患者的术中与长期预后情况。主要研究终点为3年随访时心绞痛住院、再梗塞、心力衰竭或重复血运重建和心源性死亡的复合结局。
结果显示,与非老年组患者相比,老年组患者LM病变率(25.0 vs. 15.1%,P=0.015)、3支病变率(96.4% vs. 73.8%,P<0.001)、J-CTO分≥2(36.7% vs. 23.7%,P=0.006),以及syntax积分(27.0 vs. 26.0,P=0.006)明显更高,然而两组患者的手术成功率无明显差异(69.7% vs. 82.7%, P=0.097)。3年的心源性死亡率方面,老年组明显高于非老年组(15.0% vs. 4.6%, P<0.011)。此外,老年组患者在CTO开通组与CTO未开通组3年的心源性死亡率相当(15.0% vs. 16.0%,P=1.000)。主要终点发生率无明显差异(25.0% vs. 33.0%,P=0.486)。多因素分析显示,右冠CTO、左主干病变和3支病变是老年组患者3年心源性死亡率的独立预测因子。
综上所述,该研究结果表明,老年CTOs患者冠状动脉病变严重,预后不良。CTO PCI似乎没有明显改善老年CTOs患者的长期临床结果。右冠状动脉CTO和LM疾病联合3支血管病变可能是老年CTO患者3年心脏病死亡率的独立预测因素。
原始出处:
Zhang HP, Ai H, et al., Effect of Chronic Total Occlusion Percutaneous Coronary Intervention on Clinical Outcomes in Elderly Patients. Am J Med Sci. 2018 Feb;355(2):174-182. doi: 10.1016/j.amjms.2017.09.007. Epub 2017 Sep 20.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#冠状动脉介入治疗#
37
#慢性完全闭塞#
43
#临床疗效#
37
#经皮冠状动脉介入治疗#
36
#Med#
33
谢谢梅斯提供这么好的信息,学到很多
52