患者男性,88岁,既往有心肌梗死病史曾做过冠状动脉旁路移植术,近日因双侧脚趾上的皮肤出现紫色斑驳病变到院就诊。

据该患者称,在一个月前,他曾接受过经导管主动脉瓣置换术(TAVR)。
体格检查可见,其脚趾皮肤变色(如图A和B)和网状青斑一致。
此外,实验室的检查结果显示血清肌酐水平2.8mg/dl,白细胞计数为10200/微升和嗜酸性粒细胞13%,计数为1170/微升。
取皮肤样本活检显示,可见中型动脉阻塞性胆固醇结晶,这证实胆固醇栓塞综合征的诊断(如图C、D)。
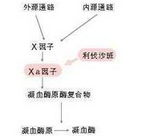
在临床上,这种综合征通常是是由远端胆固醇晶体随血管流动引起栓塞导致的,累及多个器官系统,包括外周血管,肾脏和大脑等。
一般情况下,动脉造影、血管外科手术、溶栓治疗和TAVR等容易导致该并发症的发生。
最后,该患者遵医嘱口服泼尼松和他汀类药物进行治疗。3周后,该患者脚趾上的皮肤病变明显有好转的迹象,但是,其肾功能并没有得到恢复正常。
原始出处:
Lu Devy, M.D., and Florence Brunet-Possenti, M.D. Cholesterol Embolization after Transcatheter Aortic-Valve Replacement. N Engl J Med 2016; 375:e25
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#胆固醇结晶栓塞#
34
#置换#
33
很好的内容,谢谢分享。
72
很好的内容,谢谢分享。
59
继续学习
57
继续关注
72
#主动脉瓣#
27
#主动脉瓣置换术#
24
#主动脉#
30
#经导管#
0