JACC:心脏前负荷增高可诱导肌钙蛋白的释放
2018-06-25 MedSci MedSci原创
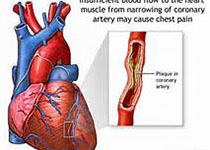
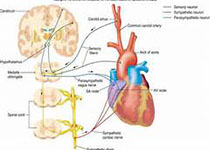
既往研究证明,心脏短暂缺血可以在不引起坏死的前提下诱导心肌肌钙蛋白I(cTnI)释放和心肌细胞凋亡。本研究的目的旨在评估左室前负荷的瞬时增高是否会在不引起心脏缺血的情况下诱导cTnI的释放。本研究对13只实验猪进行了苯肾上腺素(PE)(300 μg/min)长达1个小时的静脉注射,以增加左室舒张末期压力(LVEDP)至30mmHg,并对实验猪进行了cTnI水平和心功能的监测,心肌组织用来检测细胞凋
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#前负荷#
33
#JACC#
28
#ACC#
34
#增高#
29
#增高#
23
好文献学习了
62
临床中可以见到很多心衰的病号长期CTNI轻度升高
57