JAHA:空气污染与儿童川崎病的关系
2022-04-28 MedSci原创 MedSci原创
在这项以KD为主的全国儿童队列研究中,接触粒径≤2.5 μm的颗粒物和二氧化硫与KD的风险呈正相关。这一结果支持了环境空气污染对KD的触发作用。
川崎病(KD)是一种病因不明的全身性血管炎,主要影响5岁以下儿童。常见临床体征为发热、皮疹、红眼、红唇、颈前淋巴结肿大、关节痛。KD可导致冠状动脉瘤,是高收入国家儿童获得性心脏病的主要原因。一些研究人员提出了空气污染对KD的潜在触发效应,但由于样本量小,研究结果不一致。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员利用2007年至2019年期间的国民健康保险索赔数据,调查了韩国5岁以下人群中环境空气污染与KD之间的关联。

研究人员从235个监管监测站获取了直径≤10或2.5 μm的颗粒物、二氧化氮、二氧化硫、一氧化碳和臭氧的数据,并采用时间分层案例交叉设计,对气温和相对湿度进行调整后,根据发热当天每一种空气污染物浓度的四分位差范围增加进行条件logistic回归来估计KD的比值比(OR)。
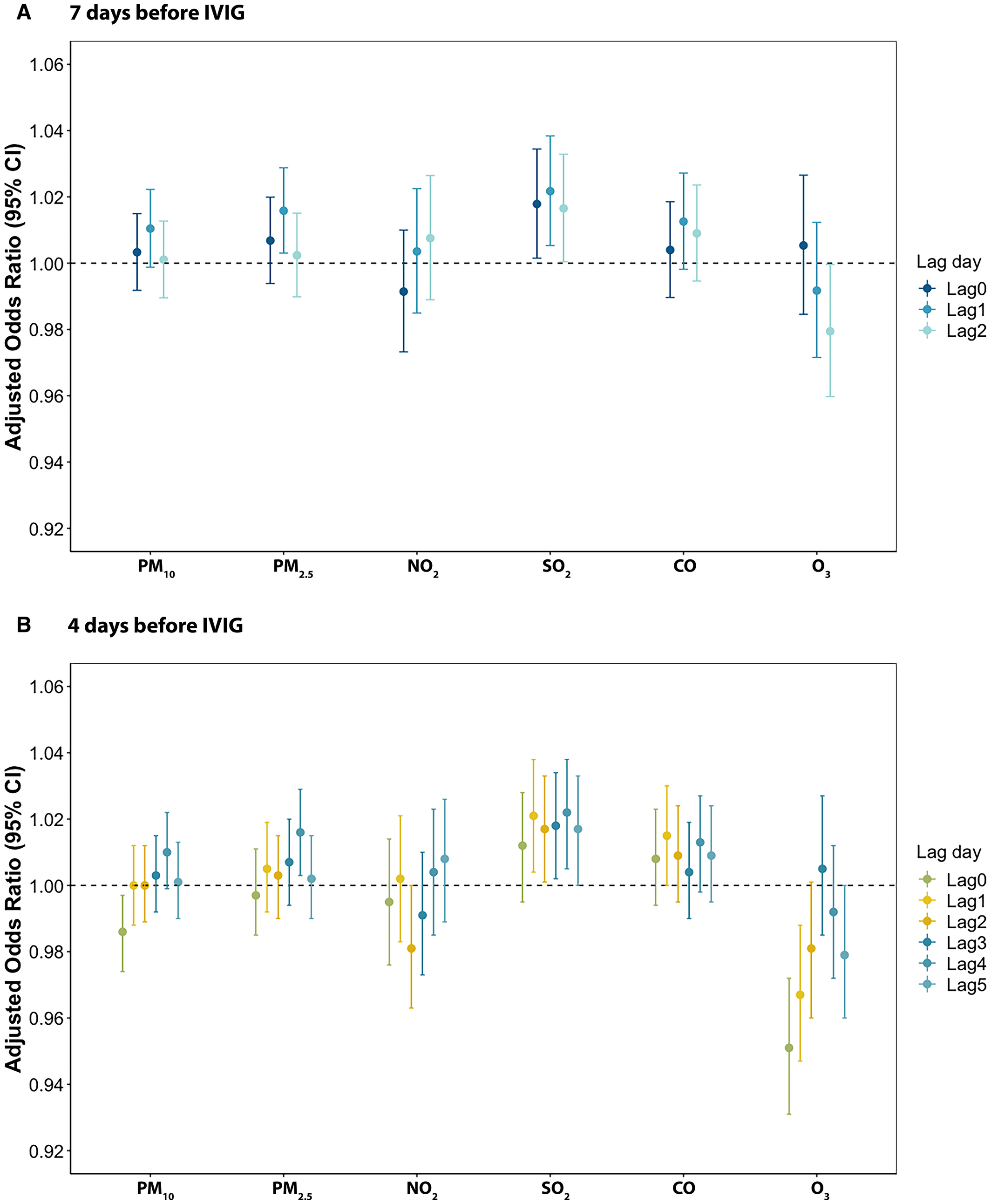
在研究期间,研究人员确定了51486名接受KD治疗的儿童。粒径≤2.5 μm的微粒浓度随着四分位范围增加(14.67 μg/m3)与滞后1时的KD呈正相关(OR为1.016;95%可信区间为1.004-1.029)。在所有滞后日,二氧化硫浓度的四分位范围内增加(2.79 ppb)与KD有关(滞后0时OR为1.018;95%CI为1.002-1.034;滞后1时OR为1.022;95%CI为1.005-1.038;滞后2时OR为1.017;95%CI为1.001-1.033)。
由此可见,在这项以KD为主的全国儿童队列研究中,接触粒径≤2.5 μm的颗粒物和二氧化硫与KD的风险呈正相关。这一结果支持了环境空气污染对KD的触发作用。
原始出处:
Dayoon Kwon.et al.Ambient Air Pollution and Kawasaki Disease in Korean Children: A Study of the National Health Insurance Claim Data.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.024092
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














学习了
52
了解了
55
#AHA#
42
#污染#
41
***
60
学到了
49