JCC:早产、分娩方式和婴儿喂养类型与儿科炎症性肠病风险无关
2022-04-12 xuyihan MedSci原创
儿童炎症性肠病的发病率近年来正在逐渐增加。如果出现不明原因的腹痛、长期拉肚子、便血,甚至是肛门周围有病变时,应提高警惕,尤其是当一般的止泻药效果不好时,更不要忽视有炎症性肠病的可能。
全球范围内,儿童发病的炎症性肠病(PIBD)的发病率正在上升,苏格兰的儿童是英国PIBD发病率最高的地区(IBD诊断年龄小于16岁),四十年来的流行病学数据证实,小儿克罗恩病的发病率增加了9倍。但在短短几十年间,PIBD发病率的大幅上升不能仅仅用遗传学来解释,还有多种原因。妊娠期和婴儿早期是对环境影响的潜在敏感期,特别是,受孕到2岁("头1000天")似乎是一个重要的窗口,在这个窗口中,遗传和环境的影响是非常大的。因此,许多围产期风险因素被认为有助于IBD的发展,可能是通过改变表观遗传学和/或微生物来实现的。本项研究旨在确定分娩方式、出生时的胎龄或6周龄时的婴儿喂养类型是否对IBD的发生有任何影响。
研究人员收集了1981 年至 2017 年间在苏格兰出生的所有儿童的临床数据,使用相关联的卫生管理数据确定胎儿的分娩方式、出生胎龄和婴儿喂养类型。PIBD 病例被定义为在 16 岁之前出现克罗恩病 [CD]、溃疡性结肠炎 [UC] 或 IBD 未分类 [IBDU]。最后使用 Cox 比例风险模型计算每次暴露的风险比 [HR]。

本项研究总共确定了 2013851名儿童,其中包括 1721 例 PIBD 病例。对编码为 CD 和/或 UC 的 261 名 PIBD 患者的验证确定 242 [93%] 为真正的IBD患者。与剖腹产相比,经阴道分娩的儿童发生 PIBD 的风险没有改变,调整后的 HR 为 0.95 [95% CI 0.84-1.08] [ p = 0.46]。与足月 [≥37 周] 出生的儿童相比,早产儿发生 PIBD 的风险没有改变,即在妊娠 24-31 周,HR 0.99 [95% CI 0.57-1.71] [ p = 0.97]在妊娠 32-36 周,HR 0.96 [95% CI 0.76-1.20] [ p= 0.71]。与 6 周时纯母乳喂养的儿童相比,纯配方喂养的儿童发生 PIBD 的风险没有改变:调整后的 HR 0.97 [95% CI 0.81-1.15] [ p = 0.69]。

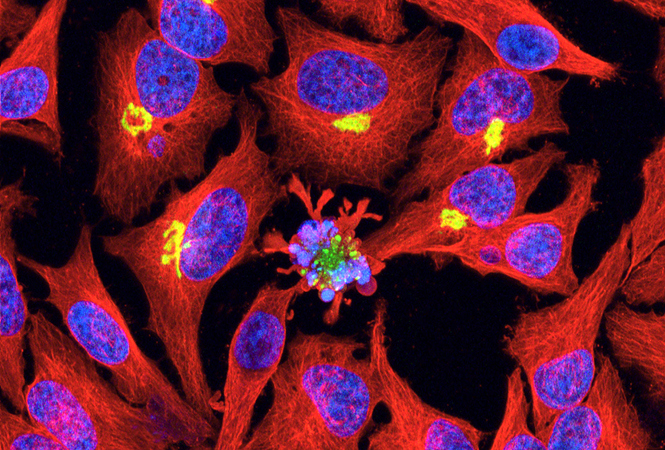
图:影响儿童炎症性肠病发展的危险因素
因此,这项基于人群的研究表明,分娩方式、胎龄或 6 周时的独家配方喂养与 PIBD 的发展之间没有关联。
原始出处:
Prematurity, Delivery Method, and Infant Feeding Type Are Not Associated with Paediatric-onset Inflammatory Bowel Disease Risk: A Scottish Retrospective Birth Cohort Study. Journal of Crohn's and Colitis.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#分娩方式#
42
#喂养#
33
好文章,值得推荐。
49
#分娩#
51
#炎症性#
34