一年一度的第71届美国心脏病学会年度科学会议(ACC 2022)已拉开帷幕,今年以线上线下的形式召开。同期,美国心脏病学会(ACC)、美国心脏协会(AHA)联合美国心力衰竭学会(HFSA)共同颁布了《2022 ACC/AHA/HFSA心力衰竭管理指南》。
新指南是对2017年指南的全面更新,包括心衰的分类、预防、诊治和合并症/共存疾病的处理,同时阐述了心衰患者的现代管理模式。本文梳理了新指南的10大核心要点,以飨读者。
核心要点1:心衰类型的新分类法
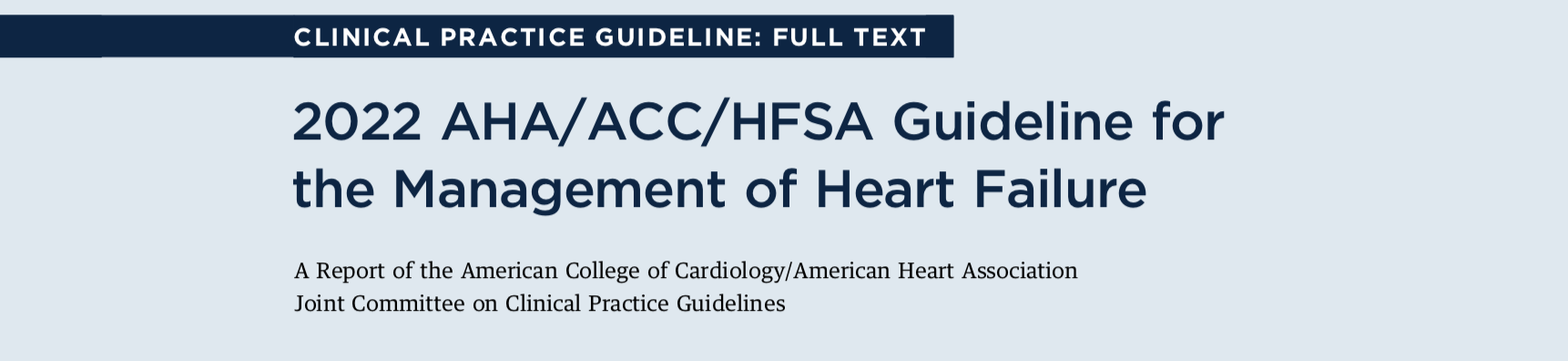
新版指南仍按照射血分数(EF)作为首次分类和再分类的标准,包括射血分数降低的心力衰竭(HFrEF)、射血分数轻度降低的心力衰竭(HFmrEF)和射血分数保留的心力衰竭(HFpEF),不同的是,新版指南强调了EF的动态演变过程,提出多次监测后再分类,增加了射血分数改善的心力衰竭(HFimpEF)。
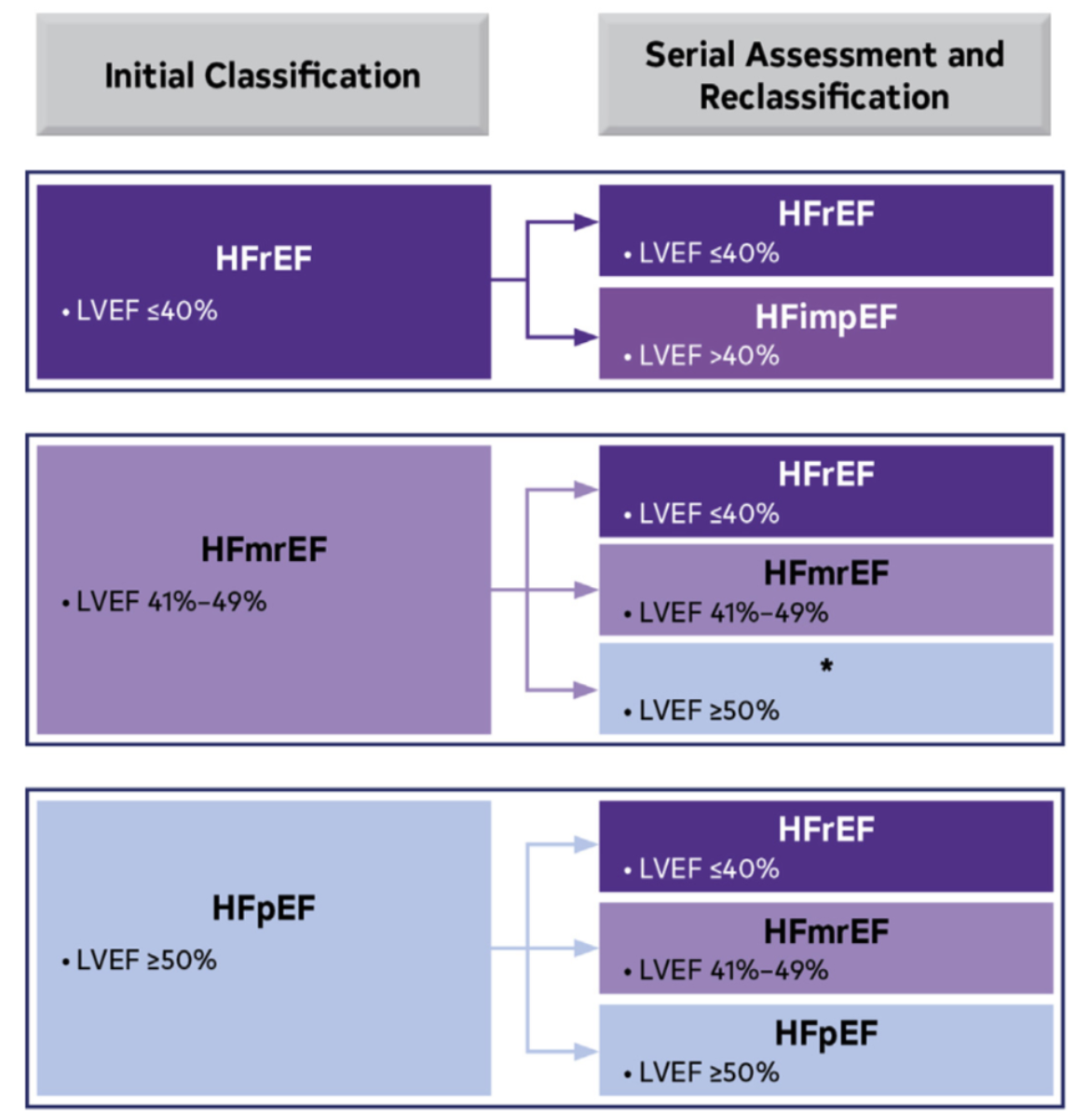
图:基于LVEF的心力衰竭分类和变化轨迹
另外,新版指南修订了心衰分期,认为应该及早识别心衰危险因素(针对A期,心衰风险期),在心脏结构变化和心功能下降发生之前提供治疗(针对B期,心衰前期)。
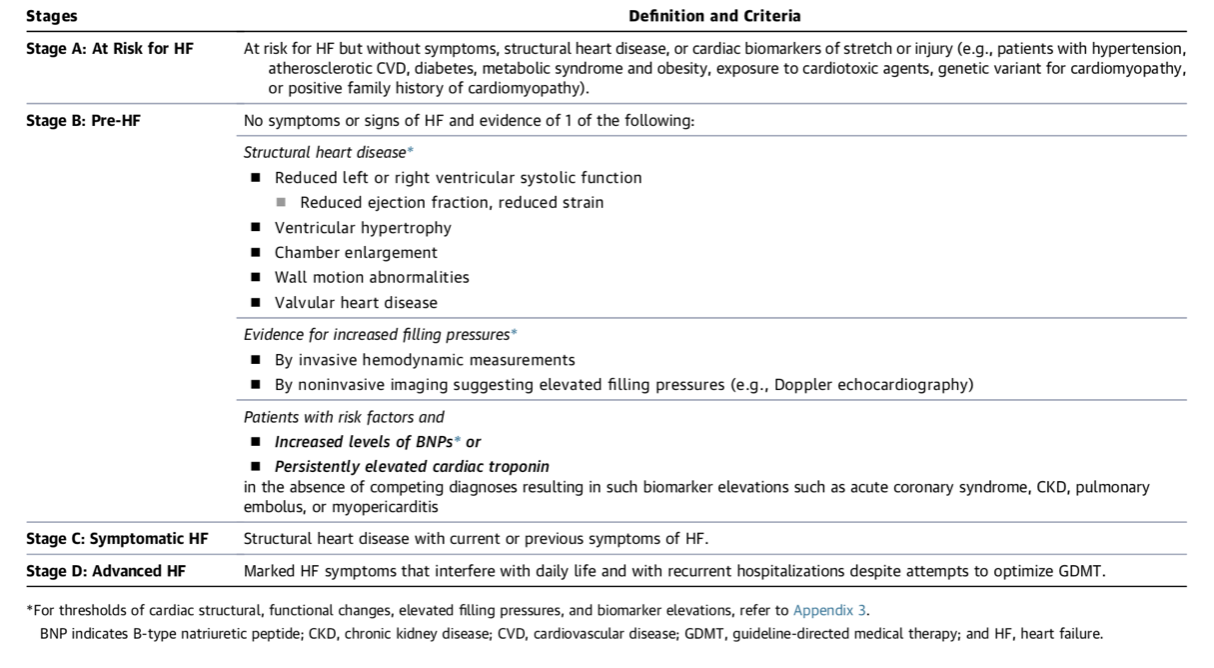
图:心衰的阶段划分、定义和标准
核心要点2:射血分数降低的心衰(HFrEF)的药物推荐
• 对于有HFrEF和NYHA II至III级患者,建议使用ARNi来降低发病率和死亡率(1,A)
• 对于以前或现在患有慢性HFrEF的患者,在使用ARNI不可行的情况下,使用ACEI有利于降低发病率和死亡率 (1,A)
•对于以前或现在患有慢性HFrEF且不能耐受ACEI的患者,当使用ARNI不可行时,建议使用ARB来降低发病率和死亡率(1,A)
•对于耐受ACEI或ARB的慢性有症状的HFrEF、 NYHA II或III级患者,建议用ARNI替代ACEI或ARB,以进一步降低发病率和死亡率(1,B-R)
•在β受体阻滞剂选择上,推荐HFrEF患者选择比索洛尔、卡维地洛、琥珀酸美托洛尔缓释剂来降低死亡率和住院率(1,A)
•对于HFrEF和NYHA II至IV级的患者,如果eGFR>30 mL/min/1.73 m2且血清钾<5.0 mEq/L,建议使用MRA(螺内酯或依普利酮)以减少发病率和死亡率。在开始使用时应仔细监测血钾、肾功能和利尿剂的剂量,并在此后密切监测,以尽量减少高钾血症和肾功能不全的风险。(1,A)
•对于有症状的慢性HFrEF患者,建议使用SGLT2抑制剂来减少住院率和心血管的死亡率,无论是否合并2型糖尿病(1,A)。
核心要点3:射血分数轻度降低的心衰(HFmrEF)药物推荐
•对于在HFmrEF患者中,SGLT-2可有利于减少住院和心血管疾病的死亡率(2a,B-R)
•对于HFmrEF(LVEF,41%-49%)的患者中,可以考虑使用β受体阻滞剂、ARNI、ACEI或ARB和MRAs来降低住院和心血管死亡的风险,特别是在LVEF处于该谱系的下限患者中(2b,B-NR)
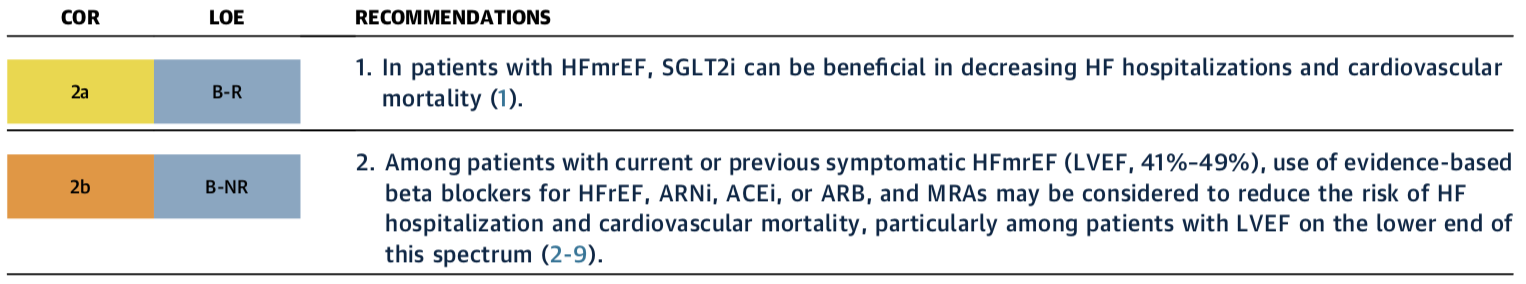
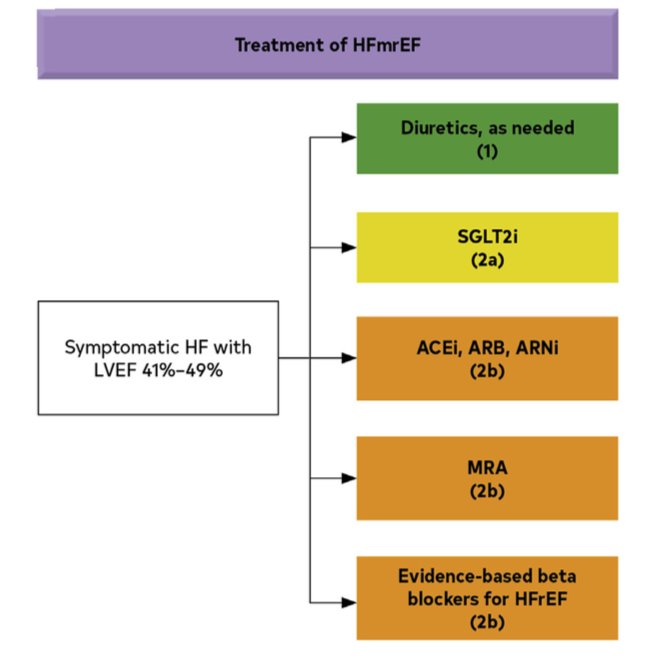
图: LVEF轻度降低(41%-49%)患者的药物治疗建议
核心要点4:射血分数保留的心衰(HFpEF)药物推荐
•在HFpEF患者中,SGLT-2可有益于减少住院和心血管疾病的死亡率(2a,B-R)
•在HFpEF患者中,可以考虑用MRA/ARB/ARNI来减少住院率,尤其是LVEF处于下限的患者(2b,B-R)
另外,在HFpEF患者中,对房颤的管理,可改善患者症状。
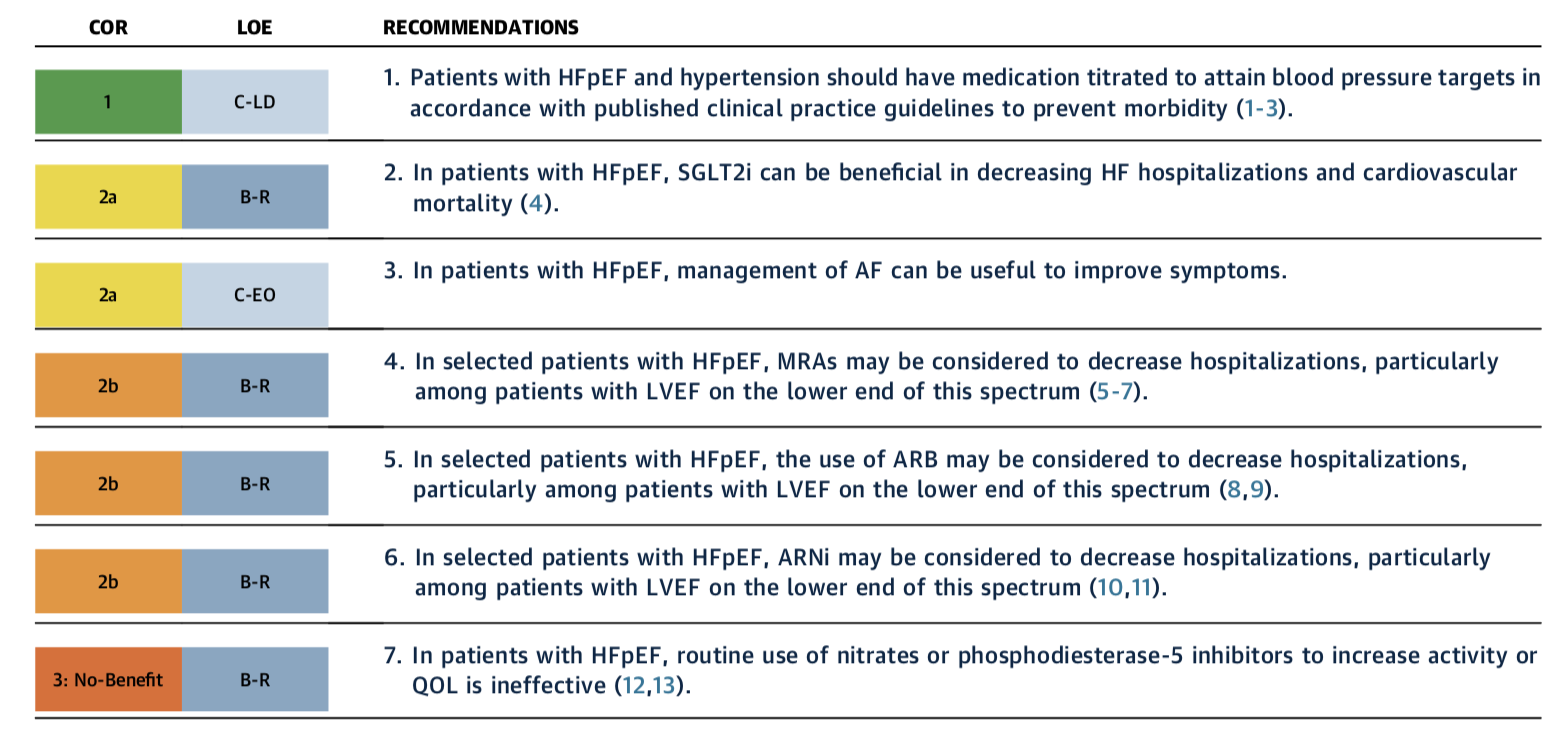
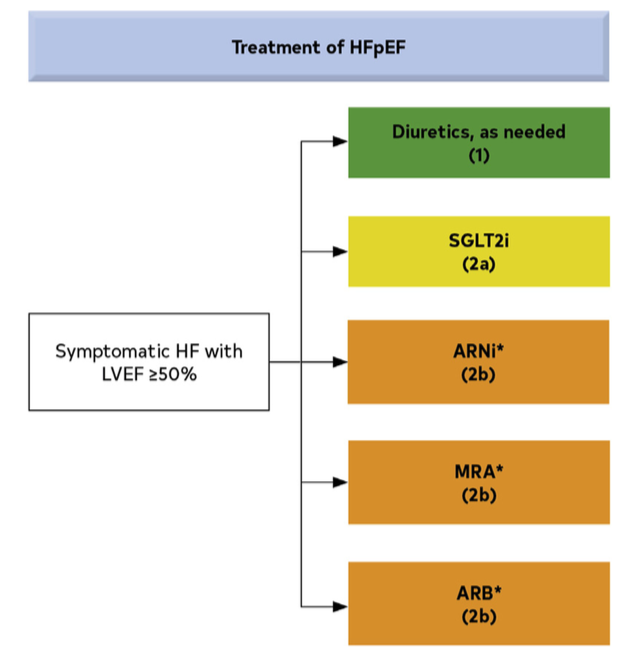
图4 HFpEF患者的药物治疗建议
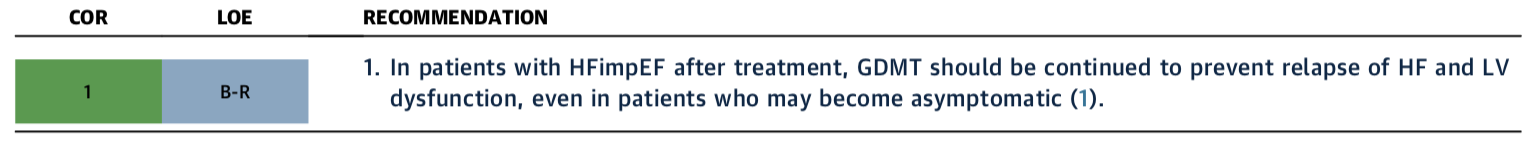
核心要点5:射血分数改善的心衰(HFimEF)药物推荐
•对于治疗后的HFimpEF患者,应继续使用GDMT以防止HF和LV功能障碍的复发,即使是那些可能变得无症状的患者(1,BR)
核心要点6:淀粉样变性心肌病新的诊断和治疗方法
•临床上,怀疑有心脏淀粉样变的患者,应通过血清和尿液免疫固定电泳和血清游离轻链进行血清和尿液单克隆轻链的筛查(1,B-NR)
• 对于临床上高度怀疑心脏淀粉样变的患者,如果没有血清或尿液单克隆轻链的证据,应进行骨扫描以确认是否存在转甲状腺素心脏淀粉样变(1,B-NR)
•对于被诊断为转甲状腺素心脏淀粉样变的患者,建议进行TTR基因测序,以区分遗传性变体和野生型转甲状腺素心脏淀粉样变(1,B-NR)
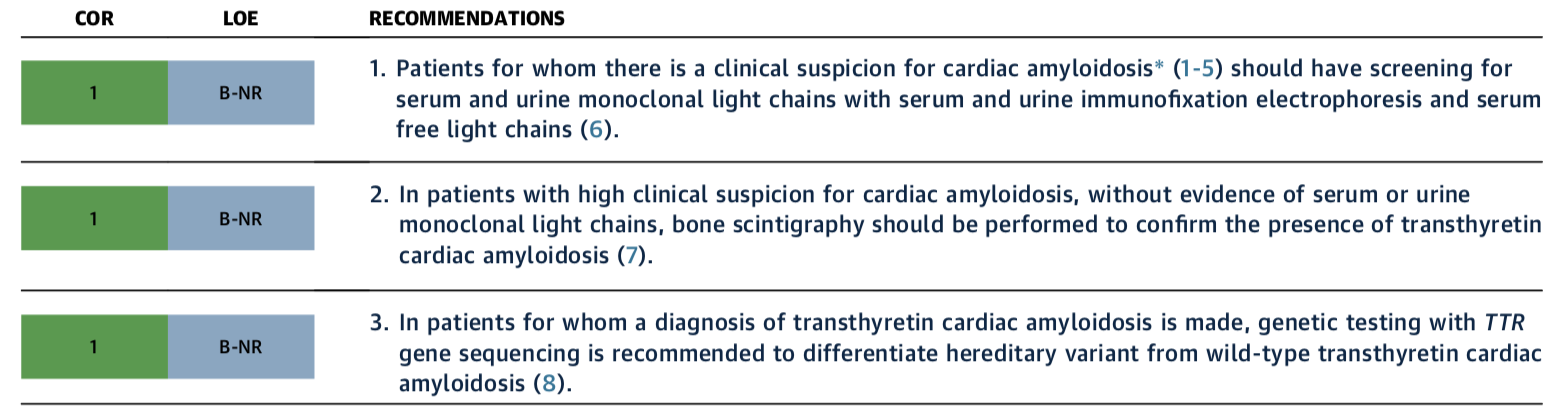
• 对于选定的野生型或变异型转甲状腺素心脏淀粉样变和NYHA I至III级HF症状的患者,转甲状腺素蛋白四聚体稳定剂治疗(tafamidis)适用于降低心血管发病率和死亡率。(1,B-R)
核心要点7:晚期心衰患者转由专业团队管理
对于晚期心衰患者,当与患者的护理目标一致时,建议及时转诊到心衰专科护理,以审查心衰管理和评估是否适合晚期心衰治疗(如LVAD,心脏移植和姑息治疗)同时,对于晚期心衰和低钠血症患者,限制液体以减少充血性症状的好处是不确定的。
核心要点8:晚期心衰患者治疗
•对于对GDMT和设备治疗难治的晚期(D期)心衰患者,如果符合条件并在等待MCS或心脏移植,持续的静脉肌力支持作为 "桥梁治疗 "是合理的(2a,B-NR)
•对于D期心衰患者,尽管有最佳的GDMT和设备治疗,但不符合MCS或心脏移植的条件,可考虑将持续的静脉肌力支持作为控制症状和改善功能状态的姑息疗法(2b,B-NR)
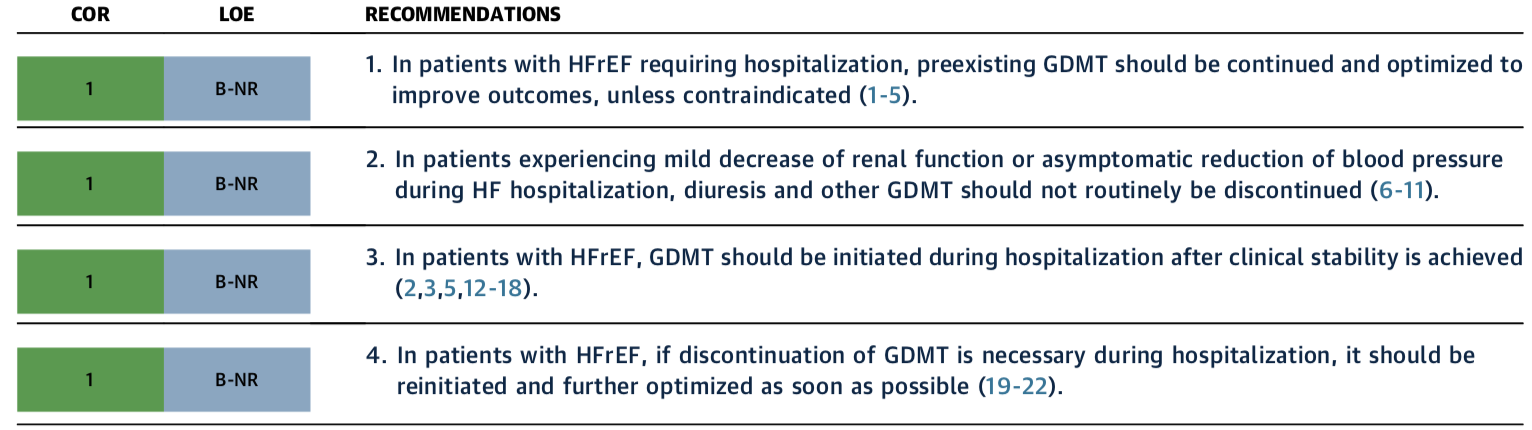
核心要点9:住院期间GDMT的维持或优化
•对于需要住院治疗的HFrEF患者,除非有禁忌,否则应继续维持和优化已有的GDMT以改善疗效(1,B-NR)
•对于高频住院期间肾功能轻度下降或无症状血压下降的患者,不应常规停止利尿和其他GDMT(1,B-NR)
•在HFrEF患者中,GDMT应在实现临床稳定后的住院期间启动(1,B-NR)
•在HFrEF患者中,如果在住院期间有必要停止GDMT,应尽快重新启动并进一步优化。
核心要点10:心衰合并症/共存病的处理和新理念
心衰的常见合并症和共病:包括心血管和非心血管病,如铁缺乏症、贫血、高血压、睡眠障碍、2型糖尿病、心房颤动、冠心病和恶性肿瘤等,新指南十分重视,提出了一些具体建议,比如,较积极地推荐射频消融术用于心衰伴心房颤动,经皮二尖瓣嵌夹术用于伴继发性二尖瓣返流(MR)患者等。
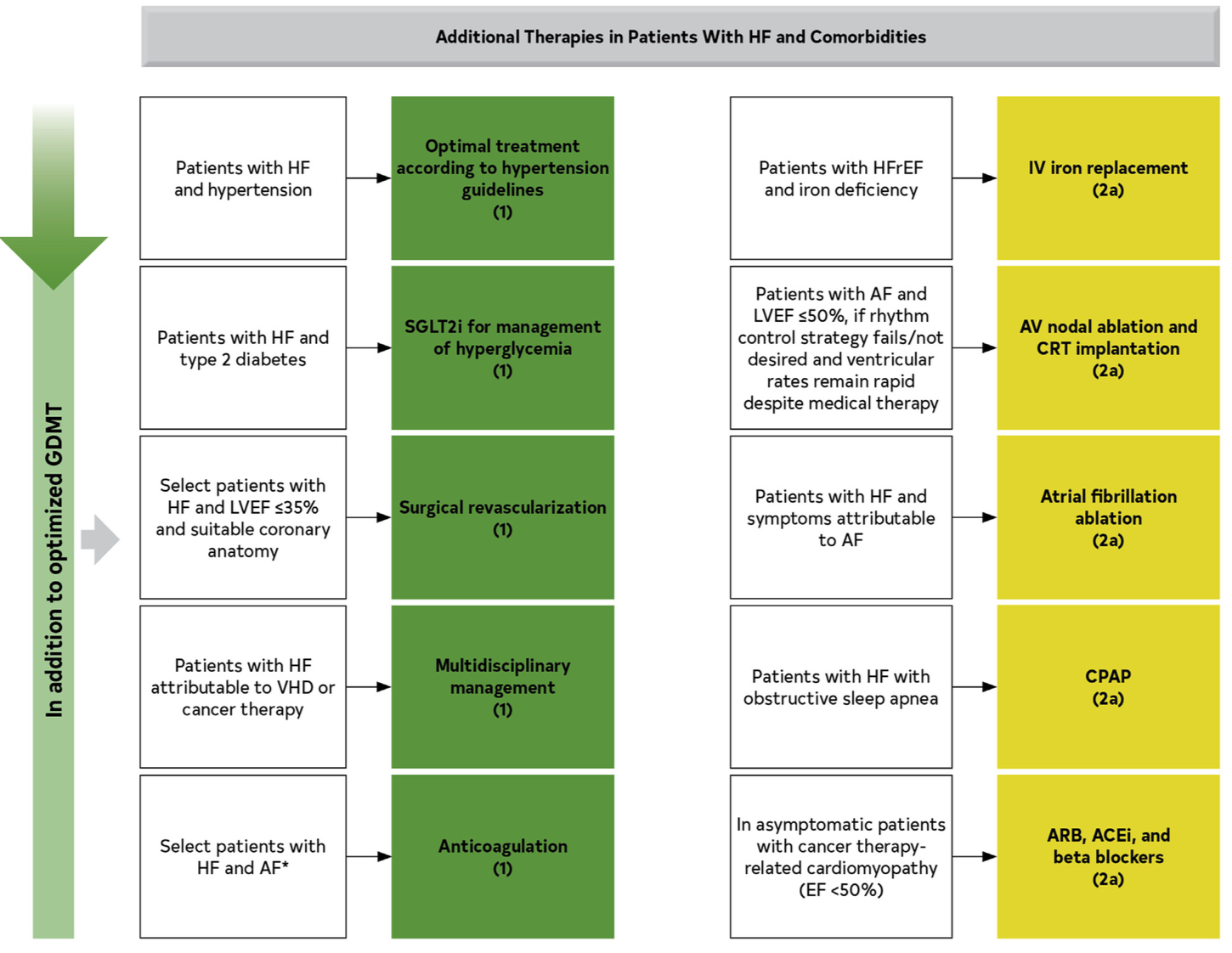
图:对特定并发症的患者的治疗建议
参考资料:
1,2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary. A Report of the American College of Cardiology/American Heart Association. J Am Coll Cardiol. 2022-4-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习.
56
#管理指南#
49
受用
60
#新定义#
50
学习了
54
#学习#
65
学习了#心血管#
76