Dig Dis Sci:溃疡性结肠炎患者门静脉血栓形成与储袋炎的关系
2022-04-27 xuyihan MedSci原创
全结直肠切除、回肠储袋肛管吻合术(ilealpouch-analanastomosis,IPAA)是UC病人的首选手术方式。掌握该手术的策略与技术要点有助于提高手术成功率、降低手术并发症。
修复性直肠结肠切除术联合回肠储袋肛门吻合术 (IPAA) 被认为是药物难治性溃疡性结肠炎 (UC)、UC 伴肿瘤或家族性腺瘤性息肉病患者的首选手术治疗方法。储袋的构造已被证明可以改善患者的生活质量并降低结肠炎相关肿瘤形成的风险。不幸的是,储袋手术的并发症很常见,例如与手术相关的漏、狭窄、窦道、瘘管和储袋炎。储袋炎是 UC 患者行 IPAA 最常见的长期并发症,据报道患病率为 23% 至 46%,年发病率为 40% 至 59%。
据推测,储袋本身结构的解剖结构改变可能会促进粪便淤滞和结肠化生,从而导致促炎环境和随后的储袋炎发生。确定发生储袋炎的风险因素可能有助于疾病的诊断和管理,并有助于规划 IPAA 的决策过程。临床经验表明,术后门静脉血栓 (PVT) 的存在可能与缺血性储袋炎有关,迄今为止,还没有发表关于基于人群的大型研究描述 PVT 和储袋炎之间的关联。本研究旨在使用基于人群的大型登记来评估储袋炎的频率和危险因素。
研究人员使用一个基于人群的数据库来搜索 1999 年至 2020 年间的接受IPAA手术患者的资料,将储袋炎患者与之前没有储袋炎的储袋构建患者进行比较。通过单变量分析确定的与储袋炎相关的因素被引入多变量模型进一步分析。事后分析进一步对 PVT 和储袋炎之间关联的人口统计学发现进行了分层分析。

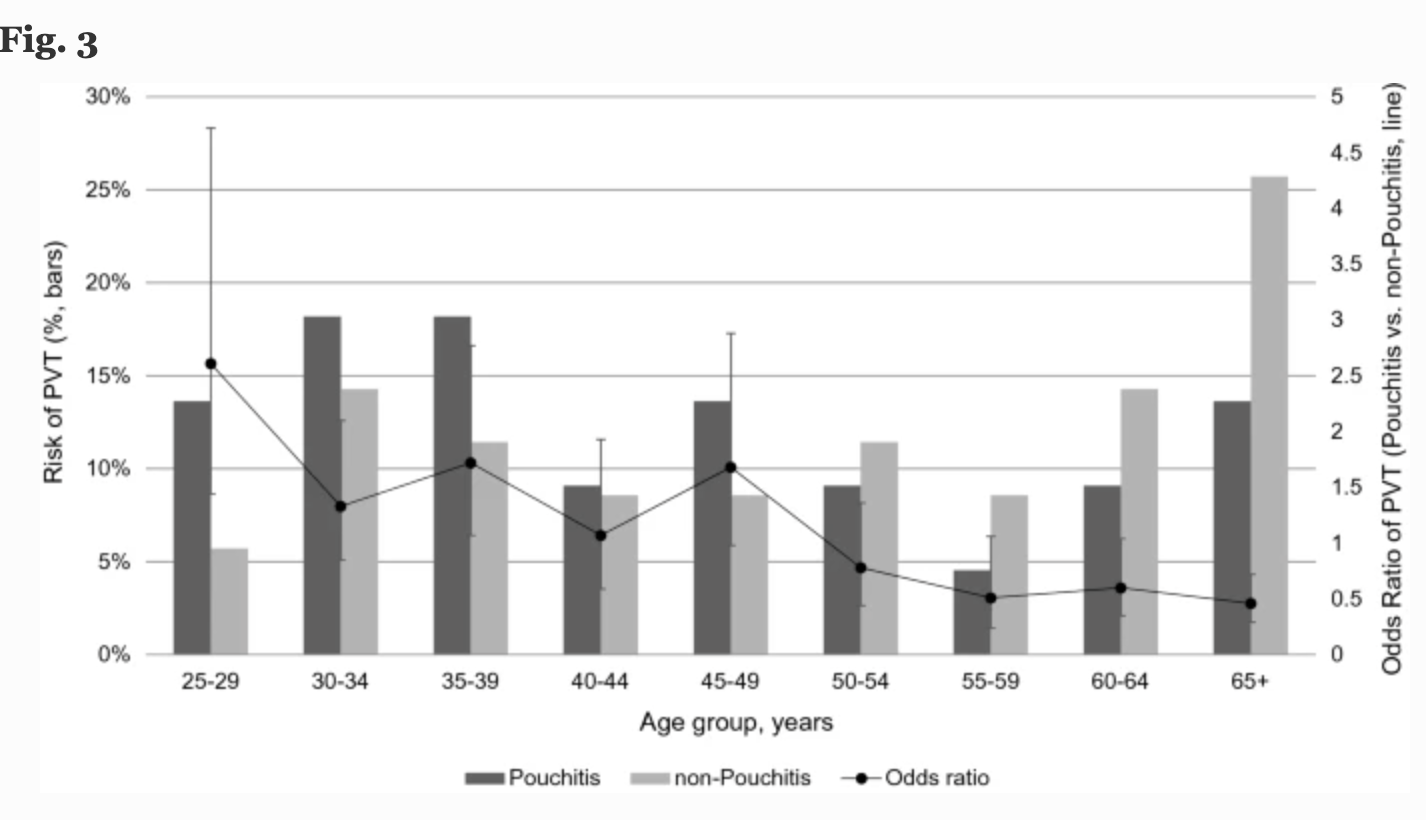
本项研究共确定了 7900 名回肠储袋炎患者(7.5%)和 97510 名没有储袋炎的患者。在多元二元逻辑回归中,PVT 患者储袋炎风险的调整优势比 (aOR) 为 10.78(95% [CI] 7.04-16.49,P < 0.001)。与储袋炎相关的其他重要因素包括男性(aOR 1.11, 95% CI 1.02–1.21, P = 0.018)、深静脉血栓形成(aOR 1.46, 95% CI 1.23–1.72, P < 0.001)和使用非甾体抗炎药(aOR 1.37, 95% CI 1.28–1.45, P < 0.001)。吸烟是一个保护因素(aOR 0.30, 95% CI 0.33–0.36, P < 0.001)。进一步的子分析显示,年轻患者患 PVT 后储袋炎患病率更高。
本项研究证实 PVT 是与储袋炎相关的独立危险因素。本项研究结果支持 PVT 作为一种潜在可控的围手术期并发症,干预PVT的发生可能会降低储袋炎的风险。
原始出处:
Aslam Syed. Et al. Association Between Portal Vein Thrombosis and Pouchitis in Patients with Ulcerative Colitis. Digestive Diseases and Sciences.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Dis#
53
#溃疡性#
46
#静脉血#
38
#门静脉血栓形成#
51
#静脉#
38
#门静脉#
52
#静脉血栓形成#
52