CGH:AGPAT1可以用来区分伴有和不伴有原发性硬化性胆管炎的溃疡性结肠炎患者
2022-04-08 xuyihan MedSci原创
原发性硬化性胆管炎(Original sclerosing cholangitis)是慢性胆汁淤积性疾病,其特征为肝内外胆管进行性炎症和纤维化,进而导致多灶性胆管狭窄。
有1%至8%的炎症性肠病(IBD)患者,尤其是溃疡性结肠炎(UC),最终将被诊断为原发性硬化性胆管炎(PSC)。由于独特的炎症行为,PSC相关的IBD被认为是一种独特的IBD表型,称为原发性硬化性胆管炎,即PSC-IBD或PSC-UC。在大多数情况下,肠道疾病比PSC的诊断要早好几年,此外,由于大多数情况下肝功能检查(LFTs)升高是转诊胆道造影的动机,PSC的诊断很可能在LFTs正常的情况下被遗漏或延误了。因此,指南主张对伴有PSC的IBD患者每年进行结肠镜检查。
最近发表的前瞻性数据表明,接受每年影像学评估的患者与不接受评估的患者相比,肝胆癌相关的死亡人数更少。随着对积极的结肠和胆道监测的支持越来越多,在IBD患者中早期发现PSC的意义也越来越大。然而,胃肠病学家仍然没有工具将PSC-IBD与"经典 "IBD群体区分开来。但是蛋白质组学为IBD的粘膜生物标志物的发现提供了希望。AGPAT1被确认为区分这两种亚型的生物标志物。因此,本项研究旨在通过研究结肠组织进行彻底的 PSC-UC 生物标志物研究。
研究人员收集了9例PSC-UC、7例UC和7例健康对照患者的福尔马林固定石蜡样本,然后收集近端结肠样本中提取蛋白质。IBD 患者均处于临床和组织学缓解期,所有UC患者均有全结肠炎病史。样品由多酶消化 FASP 处理,随后通过液相色谱串联质谱 (LC-MS/MS) 进行分析。候选蛋白质在独立队列中复制(n:PSC-UC=16,UC=21),并通过免疫组织化学(IHC)进一步验证。
在检测了所有患者的结肠蛋白组分后研究人员总共检测到了 7279 种独特的蛋白质,然后选择了基于线性回归分析的前 5 个最具差异性的蛋白质(PSC-UC 与 UC)进行进一步相关性分析。其中,AGPAT1 在 PSC-UC患者中被证实高于 UC患者 (p=0.009)。IHC 也证实了组水平的差异,与 UC 相比,PSC-UC 患者的 AGPAT1 染色更强烈。
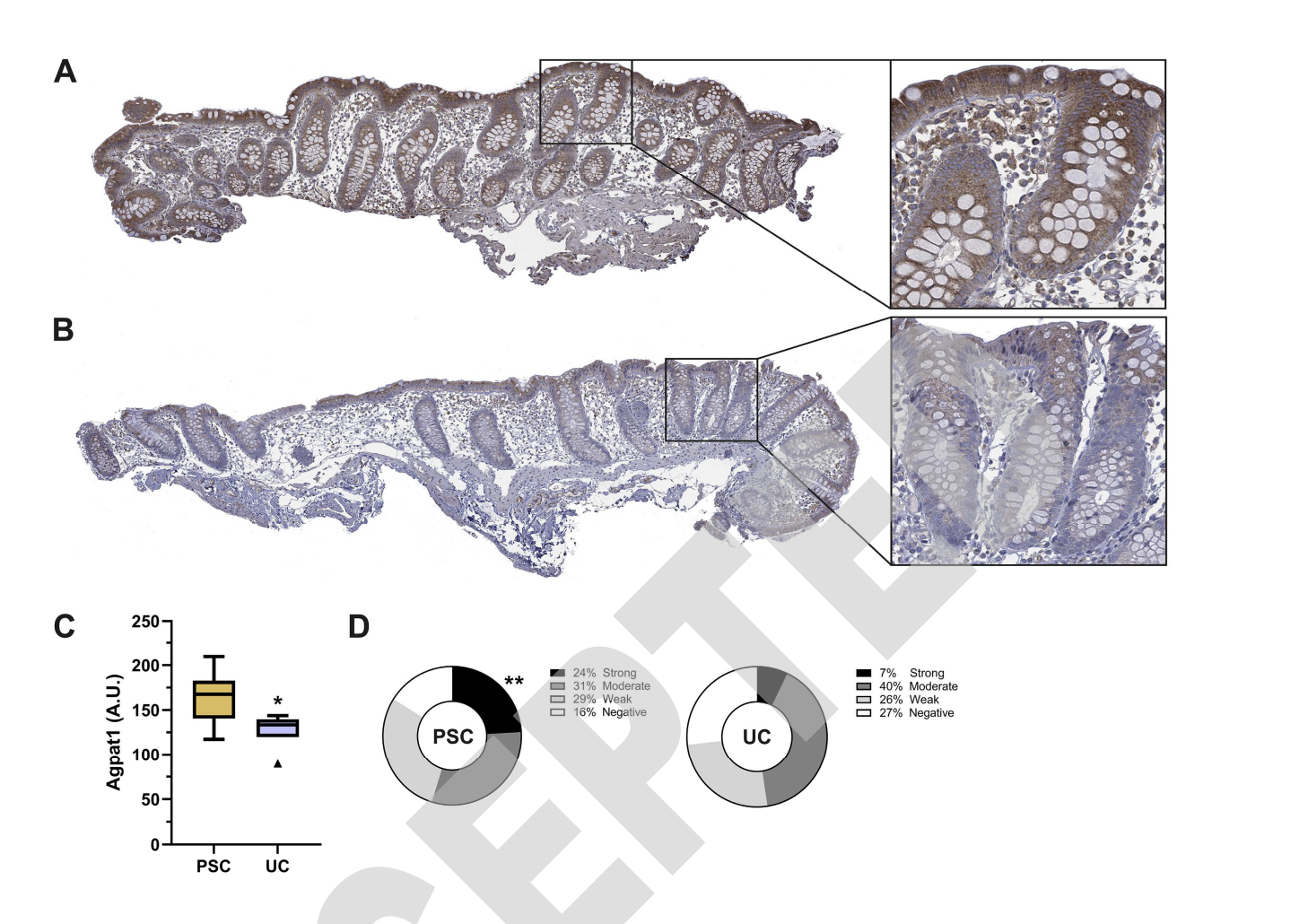
图:免疫组化染色
因此,作者最后说道,AGPAT1 这种独特的蛋白质可能可以作为区分 PSC-UC 和 UC 的潜在结肠生物标志物。本项研究结果可能对未来的 PSC-IBD 诊断和监测产生积极的影响。
原始出处:
Vessby, J. et al. AGPAT1 as a novel colonic biomarker for discriminating between ulcerative colitis with and without primary sclerosing cholangitis. Clinical and Translational Gastroenterology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CGH#
36
#原发性#
58
#溃疡性#
38
收获颇丰
44
#原发性硬化性胆管炎#
73
#硬化性#
38
#胆管#
46