NEJM:纳武单抗用于高危肌肉侵袭性尿路上皮癌根治术后辅助治疗
2021-06-03 MedSci原创 MedSci原创
高危肌肉侵袭性尿路上皮癌并接受了根治性手术的患者中,使用纳武单抗辅助治疗可显著延长患者无病生存期
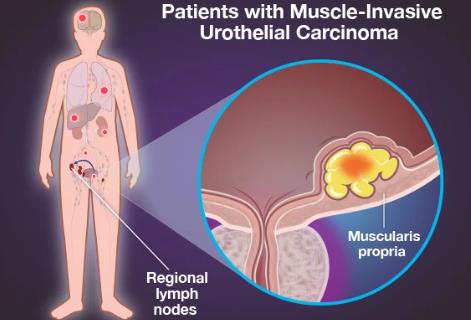
肌肉侵袭性泌尿路上皮癌患者的标准治疗为根治性手术,包括膀胱肿瘤膀胱切除术或上尿路肿瘤根治性肾切除术,但超过50%的有病理证据表明肿瘤通过固有肌肉侵入或涉及区域淋巴结的患者术后会出现转移性复发。辅助化疗对延长局部晚期患者的无病生存率有益,但其临床应用尚不普遍。近日研究人员考察了纳武单抗辅助化疗在高危肌肉侵袭性尿路上皮癌根治术后的应用效果。
本次研究为III期、多中心、双盲、随机、对照试验,接受根治性手术的肌肉侵袭性尿路上皮癌患者参与,随机每2周接受一次纳武单抗(静脉注射240mg)或安慰剂,持续1年。允许在进入试验前进行以顺铂为基础的新辅助化疗。研究的主要终点是所有患者和PD-L1表达水平为1%或以上的患者的无病生存率。次要终点为无尿路外复发生存率。
353名患者接受纳武单抗治疗,356名患者接受安慰剂。在所有人群中,纳武单抗组的中位无病生存期为20.8个月,安慰剂组为10.8个月。6个月时存活和无病的患者百分比,纳武单抗组为74.9%,安慰剂组为60.3%(疾病复发或死亡的危险比为0.70)。在PD-L1表达水平≥1%的患者中,6个月时存活和无病的患者百分比分别为74.5%和55.7%(危险比为0.55)。在所有人群中,纳武单抗组无尿路外复发的中位生存期为22.9个月,安慰剂组为13.7个月。6个月时存活且无尿路外复发的患者百分比,纳武单抗组为77.0%,安慰剂组为62.7%(尿路外复发或死亡的危险比为0.7)。在PD-L1表达水平≥1%的患者中,6个月时存活且无尿路外复发的患者百分比分别为75.3%和56.7%(危险比为0.55)。纳武单抗组的17.9%的患者出现3级或更高级别的治疗相关不良事件,安慰剂组为7.2%。纳武单抗组有两例治疗相关的肺炎死亡。

所有人群以及PD-L1阳性人群无病生存期差异
高危肌肉侵袭性尿路上皮癌并接受了根治性手术的患者中,使用纳武单抗辅助治疗可显著延长患者无病生存期。
原始出处:
Dean F. Bajorin et al. Adjuvant Nivolumab versus Placebo in Muscle-Invasive Urothelial Carcinoma. N Engl J Med,June 3,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#术后辅助治疗#
44
#侵袭性#
26
#根治术#
29
#上皮癌#
32
#根治#
22
期待OS
46
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
34