JTO:Rova-T联合纳武单抗或伊匹单抗治疗广泛期小细胞肺癌的疗效和安全性
2021-03-04 MedSci原创 MedSci原创
本研究旨在评估Rova-T联合纳武单抗或伊匹单抗用于既往治疗过的广泛期小细胞肺癌(ES SCLC)的安全性和有效性。
δ样蛋白3(DLL3)是一种在初始肿瘤细胞中表达的新型靶标蛋白,80%以上的小细胞肺癌患者会表达该蛋白。Rovalpituzumab tesirine(Rova-T)是一种靶向DLL3的抗体-药物耦合物。
本研究是一项开放的I/II期研究,旨在评估Rova-T联合纳武单抗或伊匹单抗用于既往治疗过的广泛期小细胞肺癌(ES SCLC)的安全性和有效性。
将经组织学/细胞学确诊的、既往治疗过(≥2个治疗方案)的ES SCLC患者分为两组。纳武单抗组接受0.3 mg/kg Rova-T(每6周1次,共2个疗程)+360 mg 纳武单抗(从第4周开始,2个3周疗程)。伊匹单抗组接受与纳武单抗组相同剂量的Rova-T+1 mg/kg 伊匹单抗(4个3周疗程)和1 mg/kg 伊匹单抗(第4周开始)。从第10周开始,两组患者每4周接受一次480 mg的纳武单抗治疗,主要目标是评估安全性/耐受性和有效性。
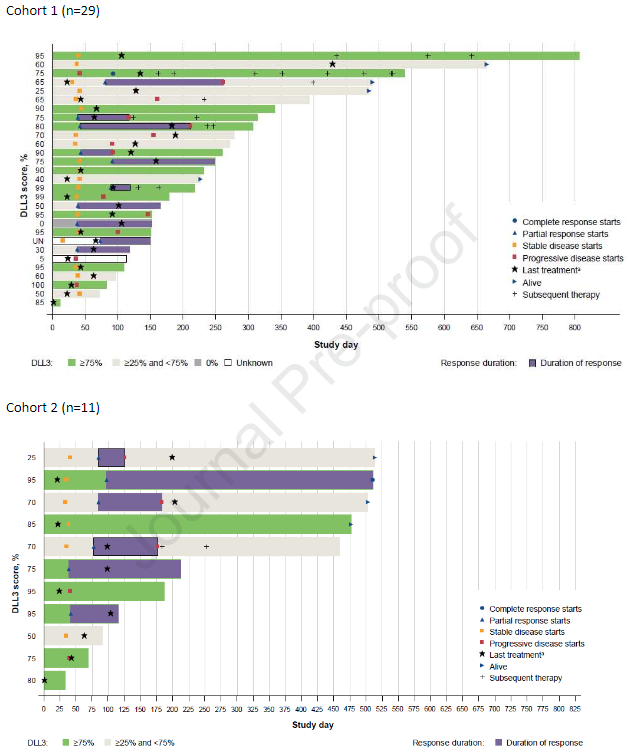
两组的治疗时间和缓解持续时间
42名患者接受了治疗:纳武单抗组 30人、伊匹单抗组 12人。总体而言,43%的患者既往接受过两种或两种以上的治疗。所有患者都经历了一次或多次需紧急治疗的不良事件(TEAE);41名患者报告了被研究者认为与研究药物有关的紧急不良事件。
最常见的TEAE为胸腔积液(n=20,48%),最常见的3级及以上的TEAE为贫血(n=9,21%)。此外,纳武单抗组还报告了3例与研究药物有关的5级TEAE:肺炎(n=2)和急性肾损伤(n=1)。
两组靶病灶的最佳百分比变化
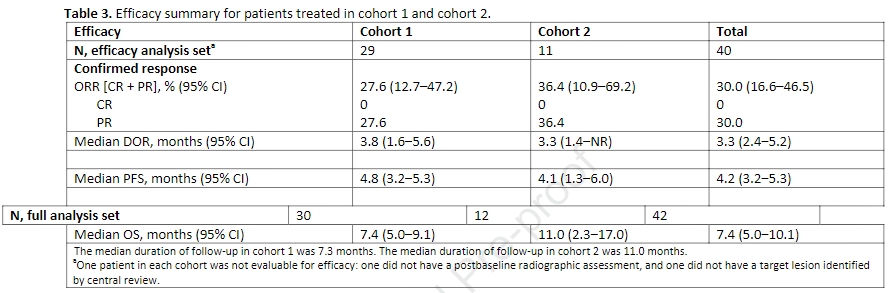
客观有效率为30%(12/40),其中纳武单抗组为27.6%(8/29),伊匹单抗组为36.4%(4/11),均为部分缓解。
疗效总结
综上,虽然Rova-T和纳武单抗或伊匹单抗的联合方案用于既往治疗过的ES SCLC患者中可获得良好的抗肿瘤活性,但患者对该研究评估的剂量水平和给药方案不能很好地耐受。
原始出处:
Malhotra Jyoti,Nikolinakos Petros,Leal Ticiana et al. A Phase I/II Study of Rovalpituzumab Tesirine in Combination With Nivolumab ± Ipilimumab in Patients With Previously Treated Extensive-Stage Small Cell Lung Cancer. J Thorac Oncol, 2021, 10.1016/j.jtho.2021.02.022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疗效和安全性#
25
#Rova-T#
29
#广泛期小细胞肺癌#
37
非常棒,谢谢分享
70
好文章!
88
谢谢梅斯提供这么好的信息,学到很多
45