JAMA子刊:静脉注射免疫球蛋白IVIG维持治疗能明显减少MOGAD复发风险,成人也一样!
2022-05-07 MedSci原创 MedSci原创
维持性IVIG与MOGAD疾病复发的减少有关。不太频繁和较低剂量的IVIG可能与治疗失败有关。
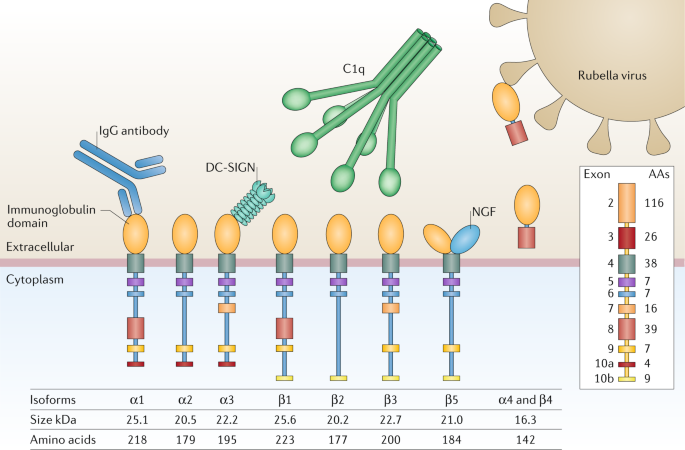
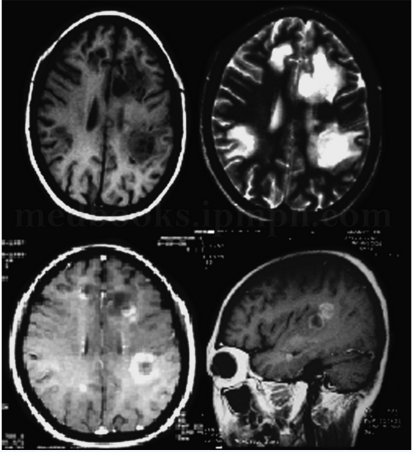
最近的研究表明,维持性静脉注射免疫球蛋白(IVIG)可能是预防髓鞘少突胶质细胞糖蛋白抗体相关疾病(MOGAD)复发的有效治疗方法;然而,这些研究大多以儿科为对象,很少有研究对成年患者的IVIG进行评估。
为了确定维持性IVIG与预防MOGAD成年患者复发的关系,来自美国mayo诊所的专家开展了一项回顾性队列研究,收集从2010年1月1日至2021年10月31日、来自9个国家的14家医院的患者。他们(1)有1次或多次符合MOGAD的中枢神经系统脱髓鞘发作史,(2)通过细胞检测法检测MOG-IgG血清阳性,以及(3)开始IVIG治疗时年龄为18岁以上。对这些患者进行回顾性评估,以了解他们是否有维持性IVIG治疗的历史。
暴露因素是维持性IVIG。主要结果是与开始治疗前相比,接受维持性IVIG治疗时的复发率。结果显示,在最初被确认为MOGAD的876名成年患者中,59人(中位数[范围]年龄,36[18-69]岁;33名女性[56%])接受了维持性IVIG治疗。15名患者(25%)开始使用IVIG作为一线免疫治疗,37名患者(63%)由于先前的免疫治疗失败,7名患者(12%)由于对先前的免疫治疗不耐受而开始使用IVIG作为二线治疗。
总的来说,IVIG治疗前的年复发率中位数(范围)为1.4(0-6.1),而接受IVIG时的年复发率中位数(范围)为0(0-3)(t108=7.14)。20名患者(34%)在接受IVIG治疗时至少有1次复发,首次复发的中位数(范围)时间为1(0.03-4.8)年,17名患者(29%)接受了伴随的维持性免疫治疗。每4周或更长时间接受1g/kg IVIG治疗的29名患者中只有5名(17%)出现疾病复发,而接受较低或较少剂量治疗的30名患者中有15名(50%)出现疾病复发(RR=3.31;95%CI,1.19-9.09)。
在最后的随访中,52名患者(88%)仍在接受维持性IVIG治疗,治疗时间中位数为1.7(0.5-9.9)年。59名患者中有7名(12%)停止了IVIG治疗:4名(57%)因疗效不佳,2名(29%)因不良反应,1名(14%)因疾病不活动期后试行不接受治疗。
这项对成年MOGAD患者的回顾性、多中心、队列研究结果表明,维持性IVIG与疾病复发的减少有关。不太频繁和较低剂量的IVIG可能与治疗失败有关。
参考文献:
Association of Maintenance Intravenous Immunoglobulin With Prevention of Relapse in Adult Myelin Oligodendrocyte Glycoprotein Antibody–Associated Disease. JAMA Neurol. Published online April 04, 2022. doi:10.1001/jamaneurol.2022.0489
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#复发风险#
37
#静脉#
34
#球蛋白#
44
#免疫球蛋白#
67
#静脉注射#
51
#MOG#
33
#IVIG#
33
JAMA上文章都是顶级的,谢谢梅斯及时上新
34