2016中国2型糖尿病合并肥胖综合管理专家共识
2016-09-02 佚名 中华内分泌代谢杂志
随着生活方式的改变及人口老龄化的加速,2型糖尿病(type 2 diabetes mellitus,T2DM)和肥胖的患病率呈快速上升趋势,并且已经成为全球性公共卫生问题。2010年中国糖尿病流行病学调查[以糖化血红蛋白(hemoglobin A1c,HbA1C)≥6.5%作为诊断标准之一]数据显示,中国成人糖尿病患病率高达11.6%,糖尿病患者人数居全球首位。肥胖和T2DM关系密切,中国超重
随着生活方式的改变及人口老龄化的加速,2型糖尿病(type 2 diabetes mellitus,T2DM)和肥胖的患病率呈快速上升趋势,并且已经成为全球性公共卫生问题。2010年中国糖尿病流行病学调查[以糖化血红蛋白(hemoglobin A1c,HbA1C)≥6.5%作为诊断标准之一]数据显示,中国成人糖尿病患病率高达11.6%,糖尿病患者人数居全球首位。肥胖和T2DM关系密切,中国超重与肥胖人群的糖尿病患病率分别为12.8%和18.5%;而在糖尿病患者中超重比例为41%、肥胖比例为24.3%、腹型肥胖[腰围≥90 cm(男)或≥85 cm(女)]患者高达45.4%。与白种人相比,中国人肥胖程度较轻,而体脂分布趋向于腹腔内积聚,更易形成腹型肥胖。
虽然既往流行病学调查中使用的超重、肥胖的诊断标准略有不同,但仍然可在一定程度上反映其高患病率,T2DM合并肥胖的管理形势非常严峻。因此,我国临床内分泌学专家根据当前中国T2DM和肥胖患者的流行病学特征及现有的临床证据,制订出本部中国T2DM合并肥胖综合管理专家共识。
一、T2DM合并肥胖管理的意义
体重增加是T2DM发生的独立危险因素。体重或腰围增加均可加重胰岛素抵抗,增加T2DM的发生风险,以及血糖控制的难度。与单纯肥胖的患者相比,T2DM合并肥胖患者减重并维持体重更加困难。首先,肥胖患者的胰岛素水平显著增高,而胰岛素具有抑制脂肪分解、促进脂肪合成的作用[8]。其次,肥胖本身与糖尿病患者存在的其他代谢异常协同作用可加重T2DM的胰岛素抵抗,而内脏脂肪增加可能是肥胖患者发生胰岛素抵抗的主要原因。减轻体重可以改善胰岛素抵抗、降低血糖和改善心血管疾病的危险因素,超重和肥胖T2DM患者减重3%~5%,即能产生血糖、HbA1C、血压、三酰甘油(triglyceride,TG)均显著降低等具有临床意义的健康获益,并且提高生活质量。在一定范围内,减重越多,获益越大。
肥胖与糖尿病存在的其他代谢异常协同作用可进一步加剧T2DM患者慢性并发症的发生。肥胖是糖尿病肾脏病变的独立危险因素,可导致慢性肾脏病的恶化。减轻体重有利于减少慢性肾脏病患者的蛋白尿,延缓肾功能衰退进程。T2DM合并肥胖使心脑血管疾病患病风险升高。因此,针对T2DM合并肥胖患者,在降糖的同时加强体重管理,对于预防糖尿病并发症、提高患者生活质量具有重要意义。
二、T2DM合并肥胖的诊断标准
目前T2DM的诊断标准与分型参考WHO 1999年标准;肥胖诊断标准参考《中国成人肥胖症防治专家共识》和《中国2型糖尿病防治指南(2013年版)》腹型肥胖的标准。符合两种疾病诊断的患者即可按照T2DM合并肥胖进行管理。糖尿病和肥胖的诊断标准见表1、表2。


三、T2DM合并肥胖的管理
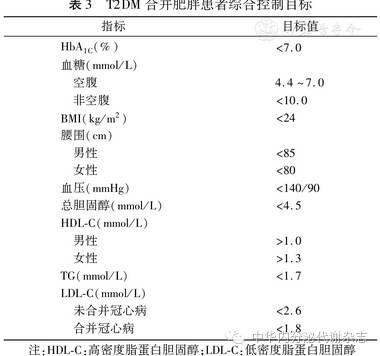
(一)T2DM合并肥胖患者的综合控制目标见表3
(二)T2DM合并超重或肥胖管理流程见图1
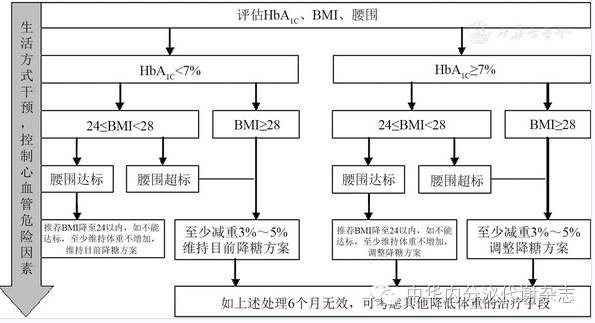
图1 T2DM合并超重或肥胖管理流程图
(三)饮食、运动和心理干预
生活方式干预应当作为所有T2DM合并肥胖治疗的基础性措施并长期坚持。
1.医学营养治疗:
(1)控制总能量。高于正常体重的T2DM患者,推荐按照25~30 kcal/(kg标准体重·d)计算,再根据患者身高、体重、性别、年龄、活动量、应激状况等调整为个体化能量标准。不推荐长期<800 kcal/d的极低能量膳食。(2)培养营养均衡的膳食习惯,蛋白质摄入量在总能量15%~20%、脂肪在总能量30%以下、碳水化合物在总能量45%~60%:①碳水化合物要注重食物品种的选择,不能单纯降低谷类主食量,以避免低血糖或酮症的发生。推荐增加低升糖指数(glycemic index,GI)食物的比例。②不建议超重或肥胖人群长期食用高蛋白质膳食;乳清蛋白有助于促进胰岛素分泌、改善糖代谢和短期内减轻体重。③应限制饱和脂肪酸与反式脂肪酸的摄入量,增加植物脂肪占总脂肪摄入的比例;膳食中宜增加富含ω-3多不饱和脂肪酸的植物油;每日胆固醇摄入量不宜超过300 mg。④保证丰富的维生素、矿物质和膳食纤维摄入,推荐每日膳食纤维摄入量为25~30 g或10~14 g/1 000 kcal。
2.运动治疗:
合理运动可改善胰岛素敏感性、骨骼肌功能、改善代谢紊乱,对改善生活质量有正反馈作用。(1)运动治疗前进行医学评估,严格把握适应证和禁忌证。(2)根据病程、严重程度、并发症等,并综合考虑年龄、家庭状况、运动习惯、文化背景等多种因素,制定个体化运动处方。运动处方应包括运动频率、运动强度、运动时间、运动类型和运动量5大要素。运动类型应以有氧运动为主。(3)注意事项:运动前、后监测血糖以预防低血糖,关键是自我监测与医师指导。如运动前血糖<4.2 mmol/L或有低血糖反应,应降低降糖药物的使用剂量。T2DM合并肥胖患者,运动时应注意预防关节疼痛和不适。
3.心理干预:
肥胖和T2DM的共存使糖尿病的治疗变得更为复杂。肥胖和糖尿病的双重压力进一步加重患者的心理负担。对于肥胖或超重的T2DM患者应该加强心理干预,通过专业心理医生或者糖尿病专科医生的心理指导,帮助患者循序渐进地改善生活方式,建立自信。降低体重不仅会减轻T2DM患者的心理障碍,而且更容易使很多患者从减肥和运动中再次获得自信,提高生活满意度。
4.药物治疗
(1)总体治疗原则:①在选择降糖药物时,应优先考虑有利于减轻体重或对体重影响中性的药物;②需要胰岛素治疗的T2DM合并肥胖患者,建议联合使用至少一种其他降糖药物,如二甲双胍、胰升糖素样肽1(glucagon-like peptide-1,GLP-1)受体激动剂(GLP-1RA)、α-糖苷酶抑制剂、二肽基肽酶4(dipeptidyl peptidase 4,DPP-4)抑制剂等,从而减轻因胰岛素剂量过大而引起的体重增加。③体重控制仍不理想者,可短期或长期联合使用对糖代谢有改善作用且安全性良好的减肥药。
(2)常用降糖药物对血糖、体重的影响:各种降糖药物的作用机制不同,对体重的影响也存在差异。T2DM合并肥胖患者在选择降糖药物时,应兼顾血糖和体重,尽可能选择降糖效果肯定同时不增加体重的药物。常用降糖药物对血糖、体重及内脏脂肪的作用见表4。
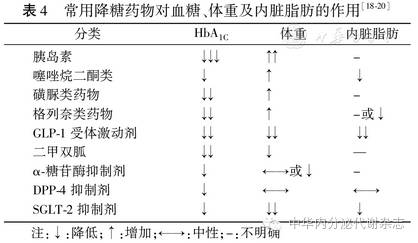
降糖同时增加体重的药物有胰岛素、噻唑烷二酮类(thiazolidinediones,TZDs)、磺脲类药物。
胰岛素仍是迄今为止最强有效的降糖药物,胰岛素的增重效应呈剂量依赖性和个体差异性,但不同胰岛素种类在增重方面有所差异,如基础胰岛素类似物——地特胰岛素具有体重增加较少的优势。TZDs主要通过增加靶细胞对胰岛素作用的敏感性而降低血糖,可使HbA1C下降1.0%~1.5%,引起体重增加(主要为水钠潴留)。
磺脲类药物通过刺激胰岛β细胞分泌胰岛素,增加体内胰岛素水平来发挥降糖作用,可使HbA1C降低1.0%~1.5%;磺脲类药物也可引起体重增加。
降糖同时减轻或不增加体重的降糖药物主要有GLP-1受体激动剂、二甲双胍、α-糖苷酶抑制剂、DPP-4抑制剂和钠-葡萄糖协同转运蛋白2(sodium-glucose cotransporter-2,SGLT-2)抑制剂。其中,GLP-1受体激动剂可显著减轻患者体重。
GLP-1受体激动剂主要通过激活GLP-1受体发挥作用,因其降糖作用具有葡萄糖浓度依赖性,因此低血糖发生率极低。利拉鲁肽无论单药或联合治疗,均能显著降低HbA1C 1.1%~1.6%,降低体重1.0~3.2 kg,持久地缩小患者腰围,且基线体重、腰围值越大,降低体重、缩小腰围的效果越显著。LEAD-2研究中,利拉鲁肽1.2 mg或1.8 mg治疗使患者内脏脂肪分别减少17.1%和16.4%。另一种GLP-1受体激动剂艾塞那肽,与利拉鲁肽头对头比较的临床研究显示,降糖效果略差,减重效果类似。此外,利拉鲁肽(3.0 mg/d)在美国、加拿大、欧盟已经被正式批准作为减肥药。
二甲双胍通过减少肝脏葡萄糖的输出和改善外周胰岛素抵抗而降低血糖,被多个国家的糖尿病诊治指南推荐为T2DM治疗一线用药。二甲双胍可降低HbA1C 1.0%~1.5%,减轻体重约1.1 kg。
α-糖苷酶抑制剂通过减慢碳水化合物在小肠上部的吸收速度而降低餐后血糖,可以使HbA1C下降0.5%~1.1%,对体重的影响呈中性或轻度减轻体重。
DPP-4抑制剂通过抑制DPP-4活性减少GLP-1在体内的失活,使内源性GLP-1水平升高,促进葡萄糖依赖的胰岛素分泌和抑制胰升糖素分泌,可降低HbA1C 0.4%~1.0%。DPP-4抑制剂对体重的影响呈中性。
SGLT-2抑制剂主要通过减少肾脏对葡萄糖的重吸收、增加葡萄糖排泄而降低血糖水平。SGLT-2抑制剂可使HbA1C降低0.5%~1.0%,同时减轻患者体重(平均减少1.8 kg)。由于SGLT-2抑制剂增加尿糖排出,会导致代偿性的食欲旺盛,故其减重作用需要配合控制饮食或其他类似手段。
四、手术治疗
对于采取非手术治疗后减重或血糖控制效果不理想的T2DM合并肥胖患者,可以考虑手术治疗。减重手术可以改善T2DM合并肥胖患者的血糖控制,甚至使部分患者糖尿病"缓解" 。手术治疗T2DM的前提是患者尚具备足够的胰岛β细胞功能。严格选择患者及适合的手术方式,充分进行术前评估和术前准备,并加强术后随访和营养、运动指导,是提高手术治疗T2DM有效性和安全性的关键。
(一)适应证
1.年龄在18~60岁,一般状况较好,手术风险较低,经生活方式干预和各种药物治疗难以控制的2型糖尿病患者(HbA1C>7.0%)。
2.根据患者的BMI和临床情况来判断是否行手术治疗:(1)积极手术:BMI≥32 kg/m2,无论是否存在其他合并症(阻塞性睡眠呼吸暂停综合征、非酒精性脂肪性肝炎、高尿酸血症、多囊卵巢综合征、肾功能异常等);(2)慎重手术:BMI 28~32 kg/m2,至少符合额外的2个代谢综合征组分,或存在合并症;(3)暂不推荐:BMI 25~28 kg/m2。如果患者合并腹型肥胖,且至少符合额外的2个代谢综合征组分,可酌情提高手术推荐等级。
腹腔镜袖状胃切除术(laparoscopic sleeve gastrec-tomy,LSG)是中重度T2DM合并肥胖的首选术式;胃旁路术(roux-en-Y gastric bypass,RYGB)适用于T2DM病程相对较长、需要减重更多的患者。
(二)禁忌证
1.滥用药物、酒精成瘾、患有难以控制的精神疾病患者,以及对减重手术的风险、益处、预期后果缺乏理解能力的患者。
2.明确诊断为1型糖尿病的患者。
3.胰岛β细胞功能已明显衰竭的2型糖尿病患者。
4.外科手术禁忌者。
5.BMI<25 kg/m2。
6.妊娠糖尿病及其他特殊类型的糖尿病。
五、血糖和体重监测
(一)血糖监测
HbA1C反映近2~3个月血糖平均水平,是评价长期血糖控制的金标准,也是指导临床调整治疗方案的重要依据。在治疗初期建议每3个月检测1次,一旦达到治疗目标可每6个月检查一次。
(二)体重监测
1.作为一种慢性疾病,为了预防体重再次增加和防治并发疾病,体重长期监测必不可少。
2.有效性评估:建议糖尿病合并肥胖患者体重降幅至少>3%。采用药物治疗3个月后对疗效进行评价:体重下降2%~3%为不显著;体重下降3%~5%为显著;体重下降>5%为非常显著。
3.在6个月时间达到5%~15%的体重下降;重度肥胖(如BMI>35 kg/m2)可能需要更多(20%或以上)的体重减轻。
4.对于接受手术治疗的患者,在术后第1年至少要进行3次门诊随访,还需要更多的电话或其他方式的随访。对于可调节胃绑带术的患者,门诊随访的次数可能需要增加,以便对绑带进行适当的调节。
六、T2DM合并肥胖心血管风险因素的控制
T2DM及肥胖确诊后,至少每年评估一次心血管病变的风险因素,评估的内容包括心血管病既往史及现状、年龄、有无心血管风险因素(吸烟、血脂紊乱、高血压和家族史等)、肾脏损害(尿白蛋白排泄率增高等)、心房颤动(可导致卒中)。全面评估和控制心血管疾病风险因素,并进行合理的降压、调脂和抗血小板治疗,可显著改善糖尿病患者心脑血管病变和死亡发生的风险。联合使用其他药物时应注意:β受体阻滞剂增加体重、他汀类药物升高血糖、某些抗抑郁焦虑药物增加体重等。
共识下载:
2016 中国2型糖尿病合并肥胖综合管理专家共识(点击即可下载)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#专家共识#
32
#综合管理#
33
文章很好,非常有益
0
学习了。。。
75
都是好东西,认真学习,感谢无私的付出
59
很好,不错,以后会多学习
0
继续学习
79
继续关注
34
加油共识们
22