Cell:艾滋病病毒如何悄然跨越粘膜屏障和免疫屏障?
2016-04-17 何嫱 生物通
一项新研究通过观测接触了SIV(HIV相似物)的猴子,揭示出了在血液中可以检测出病毒之前,感染最早阶段发生的事件,这是一个在人类中至关重要但又难于研究的时期。发表在《细胞》(Cell)杂志上的研究结果对于开发疫苗及其他的感染预防策略具有重要的意义。 领导这一研究的是哈佛医学院医学教授、贝斯以色列女执事医疗中心(BIDMC)病毒学与疫苗研究中心主任Dan Barouch博士。近年,Barouch领
一项新研究通过观测接触了SIV(HIV相似物)的猴子,揭示出了在血液中可以检测出病毒之前,感染最早阶段发生的事件,这是一个在人类中至关重要但又难于研究的时期。发表在《细胞》(Cell)杂志上的研究结果对于开发疫苗及其他的感染预防策略具有重要的意义。
领导这一研究的是哈佛医学院医学教授、贝斯以色列女执事医疗中心(BIDMC)病毒学与疫苗研究中心主任Dan Barouch博士。近年,Barouch领导研究团队在艾滋病研究中取得一系列重要的研究成果。

Barouch说:“在接触病毒后的最初几天,可以初步检测到血液中的病毒之前所发生的事件对决定感染过程起至关重要的作用,但在人类基本上不可能去研究这一时期。到目前为止我们的研究最全面地评估了急性HIV/SIV感染。”
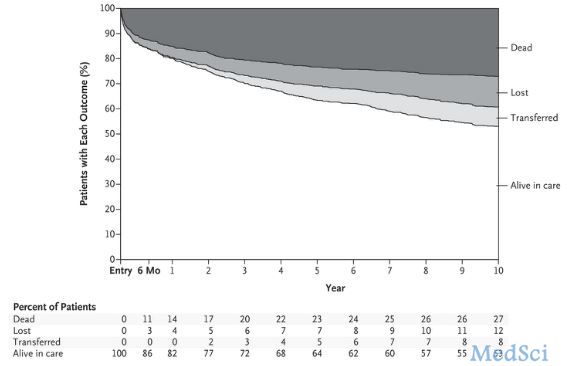
当Barouch和同事们让44只猕猴接触SIV,并在接触病毒后的0, 1, 3, 7和10天进行动物分析时,他们发现SIV可以迅速传播至全身,在接触病毒24小时后分析的大多数猴子中,病毒RNA存在于除生殖系统之外的至少一种组织中。
Barouch说:“除了快速的传播,病毒还触发了局部的炎症反应,它似乎抑制了抗病毒天然和适应性免疫,因此有可能扩大了自身的复制。这些数据提供了有关感染最早期事件的一些重要认识。”
这种炎症反应发生在接触SIV后不久的病毒感染组织中,病毒RNA量增加与宿主蛋白NLRX1升高有关联,NLRX1抑制了抗病毒免疫反应。此外,还触发了抑制适应性免疫反应的TGF-β细胞信号通路(它与低水平的抗病毒T免疫细胞反应相关联)及较高水平的SIV复制。研究人员观察到早在接触病毒后1天,包含病毒RNA的组织中TGF-β信号通路中的一些基因表达即升高。
研究结果表明,有可能存在一个非常狭小的机会窗来抑制或清除病毒。HIV预防策略应该将这些因素考虑在内。Barouch 说:“我们相信这些有关早期HIV/SIV感染的新认识,对于开发出诸如疫苗、抗体、杀微生物剂和药物等一些干预措施来阻断感染至关重要。这条研究线路的下一步是评估各种干预对这些早期事件有可能产生的影响。”
最近另一项研究表明,在艾滋病病毒感染早期,脾脏内 Tfh细胞出现早期丢失现象,使得机体对HIV病毒的防御能力暂时性丢失,文章发表在PLoS Pathog上,这些都表明,HIV早期接触人体时,会产生一系列抑制人体防御能力的措施。
2013年,Barouch领导的一个研究小组证实一组近期发现的抗体或许可以高效治疗HIV。他们的研究结果发表在Nature杂志上,将推动研发这些单克隆抗体作为人类的艾滋病新疗法(Nature:单克隆抗体或能有效治疗艾滋病)。2014年,Barouch证实在猕猴直肠内感染猴免疫缺陷病毒(SIV)之后,可检测到病毒血症之前的极早期病毒储存库就已建立起来。这些结果在线发表在Nature杂志上(Nature:HIV感染者体内病毒储存库的建立极早)。2015年,Barouch领导的一项新研究显示,一种新型HIV-1疫苗疗法为一半接种疫苗的非人灵长类动物(NHPs)提供了完全防护,对抗了SIV连续6次反复的攻击。这些研究结果发布在Science杂志上(艾滋病重大研究进展速览)。美国哈佛大学医学院等机构的研究人员的开发出了一种拼接多种基因的“马赛克疫苗”。动物试验显示,该疫苗可使艾滋病病毒感染风险降低约90%。这一研究成果有可能为人类“防艾”带来新希望(Cell:“马赛克疫苗”临床前研究表明能降低艾滋病感染风险90%)
原始出处:
Dan H. Barouch, Khader Ghneim, William J. Bosche, Yuan Li, Brian Berkemeier, Michael Hull, Sanghamitra Bhattacharyya, Mark Cameron, and others. Rapid Inflammasome Activation following Mucosal SIV Infection of Rhesus Monkeys.DOI: http://dx.doi.org/10.1016/j.cell.2016.03.021
Moukambi F, Rabezanahary H, Rodrigues V, Racine G, Robitaille L, Krust B, Andreani G, Soundaramourty C, Silvestre R, Laforge M, Estaquier J.Early Loss of Splenic Tfh Cells in SIV-Infected Rhesus Macaques. PLoS Pathog. 2015 Dec 7;11(12):e1005287.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#粘膜#
28
#CEL#
26
#Cell#
24
#膜屏障#
33
#免疫屏障#
43
#艾滋病病毒#
27
来学习!!!
100
不知道?????
93