JACC:氯吡格雷可有效治疗非ST段抬高型心肌梗死
2014-06-11 坞霜降 丁香园
尽管临床试验结果显示在不稳定心绞痛(UA)或非ST段抬高型心肌梗死(NSTEMI)患者治疗药物中,氯吡格雷具有降低心血管疾病(CV)发病率及死亡率的效果,但是有必要进一步评估氯吡格雷在实际临床工作中的治疗效力。 因此,Matthew D. Solomon博士等人从临床实际出发评估了氯吡格雷的效力,其研究结果发表于Journal of the American College of Cardi
尽管临床试验结果显示在不稳定心绞痛(UA)或非ST段抬高型心肌梗死(NSTEMI)患者治疗药物中,氯吡格雷具有降低心血管疾病(CV)发病率及死亡率的效果,但是有必要进一步评估氯吡格雷在实际临床工作中的治疗效力。
因此,Matthew D. Solomon博士等人从临床实际出发评估了氯吡格雷的效力,其研究结果发表于Journal of the American College of Cardiology杂志。【原文下载】
该回顾性队列研究选取了北加州凯萨医疗机构的患者,条件为无冠脉疾病病史、无氯吡格雷服用史、于2003年至2008年间出现UA或NSTEMI,同时研究者依照CUER研究排除了有卒中病史或短暂性脑缺血病史的患者。
在2年的随访中,研究者采用倾向型匹配多变量Cox分析法评估了氯吡格雷治疗与全因死亡率、因心梗入院情况及死亡心梗复合事件之间的关系。
该研究入组患者例数16365。36%的患者在出院7天内嘱给予氯吡格雷治疗。8562例患者的倾向匹配分析结果显示使用氯吡格雷后的因死亡率及心梗复合事件发生率较低,但心梗发生率并未降低。
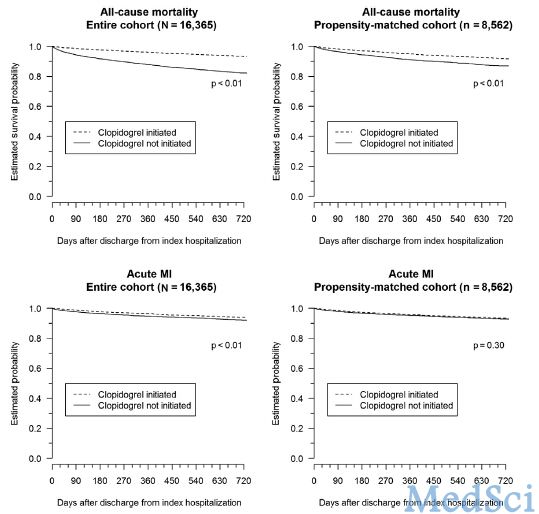
此次大型社区基础的患者研究结果显示,氯吡格雷与心梗及死亡的综合发生率降低相关,而且这种相关性在NSTEMI患者群体尤为明显。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
33
#非ST段抬高型心肌梗死#
39
#非ST段抬高型#
28
#非ST段#
36
#非ST段抬高#
25
#ACC#
27
#ST段抬高#
42
#有效治疗#
29
#ST段#
30