J Autoimmun:接种SARS-CoV-2疫苗后引发的弥漫性-皮肤型系统性硬化症
2022-03-25 小文子 MedSci原创
研究报告第一例由SARS-CoV-2疫苗引发的SSc病例。
Journal of Autoimmunity杂志最近报告了一例70岁男性弥漫性-皮肤型系统性硬化症(SSc),患者在接种首剂ChAdOx1 nCOV-19疫苗两周后发生快速进展性皮肤增厚。

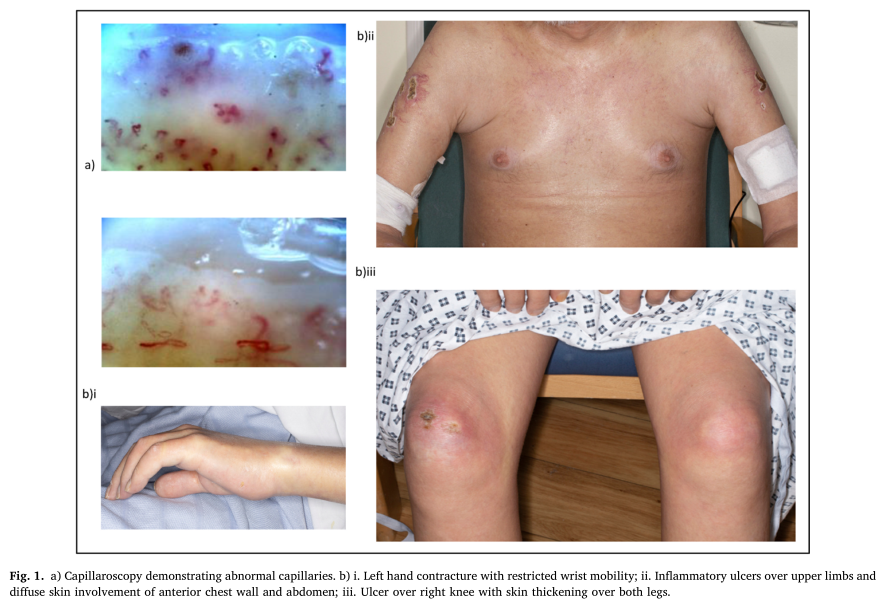
患者在接种疫苗之前没有SSc的特征,目前吸烟,有肺气肿征象,未接触任何已知的有毒化合物。初始症状出现6个月后评估以下项目。根据改良Rodnan皮肤评分(mRSS)47/51,皮肤评分高,近端肢体有多处炎症性溃疡。患者无手指雷诺现象,溃疡没有影响其手指,然而甲襞毛细血管镜检查证明毛细血管迂曲,轻度扩张和脱落。肌电图显示活动性肌炎。肌钙蛋白T(82 ng/L)和脑钠肽(744 ng/L)升高,与心肌炎临床表现程度一致。
由于患者SSc的发病时间与第一剂疫苗的接种时间非常接近,没有其他触发因素,因此怀疑ChAdOx1 nCOV-19疫苗可能存在不良反应。
研究人员假设编码SARS-CoV-2棘突蛋白抗原的重组腺病毒载体触发了非预期的免疫激活,导致ANA阳性、ENA阴性亚组患者出现非典型迟发性SSc。
接种SARS-CoV-2疫苗后,报告了大量炎症不良事件(AE),从短期或局部炎症事件到长期自身免疫性疾病的发展。这种情况下发生自身免疫的机制可能包括分子模拟和“旁观者效应”。如果疫苗核蛋白/刺突蛋白和自身抗原的共享肽序列导致自身抗体形成,则可发生分子模拟。伴随的理论是,病毒刺突蛋白或疫苗固有佐剂活性可能传递抗原信号,抗原提呈细胞异常激活并产生促炎介质。靶向SSc相关自身抗原的IgG自身抗体在COVID-19感染中被鉴定。值得注意的是,这些自身抗体在时间上与抗SARS-COV-2 IgG应答相关,提示在COVID-19感染和疫苗应答的发病机制中具有潜在的广泛B细胞应答。
研究报告了第一例由SARS-CoV-2疫苗引发的SSc病例。然而,探索SARS-COV-2疫苗与感染之间自身免疫的共同机制可进一步了解SSc的病因和发病机制。
原文出处:
Alice Cole, Rhys Thomas, Nina Goldman, et al, Diffuse cutaneous systemic sclerosis following SARS-Co V-2 vaccination, Journal of Autoimmunity, 2022, https://doi.org/10.1016/j.jaut.2022.102812.

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#系统性#
39
#硬化症#
41
#SARS-CoV#
49
#皮肤型系统性硬化症#
44
#SARS#
38
#弥漫性#
45
#系统性硬化#
34