Leukemia:CXCR4的过度激活驱动慢性淋巴细胞白血病的发生发展
2021-08-10 xiaozeng MedSci原创
CXCR4是一种G蛋白偶联受体,其可调节造血干细胞的稳态、骨髓的生成、淋巴细胞的生成以及驱使免疫细胞向其配体CXCL12接近的趋向作用。
CXCR4是一种G蛋白偶联受体,其可调节造血干细胞的稳态、骨髓的生成、淋巴细胞的生成以及驱使免疫细胞向其配体CXCL12接近的趋向作用。
既往研究显示,CXCL12的结合可诱导多种G蛋白依赖性和非依赖性信号通路,包括PI3K/AKT、MAPK/ERK和PLC/Ca2+信号通路。而异常的CXCR4活性与淋巴瘤的发生发展以及治疗抗性相关。
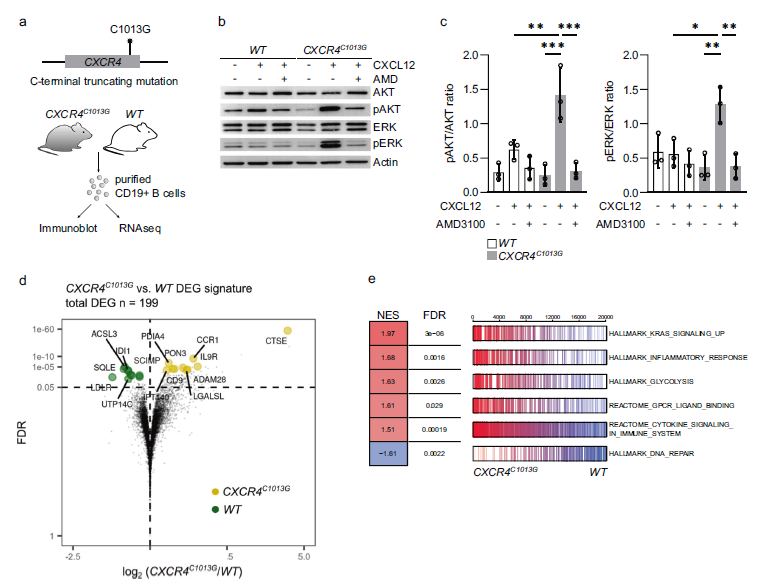
在该研究中,研究人员构建了具有CXCR4信号过度激活的功能获得性CXCR4突变(CXCR4 C1013G)小鼠模型,并鉴定CXCR4为多个关键致癌途径的关键激活因子。
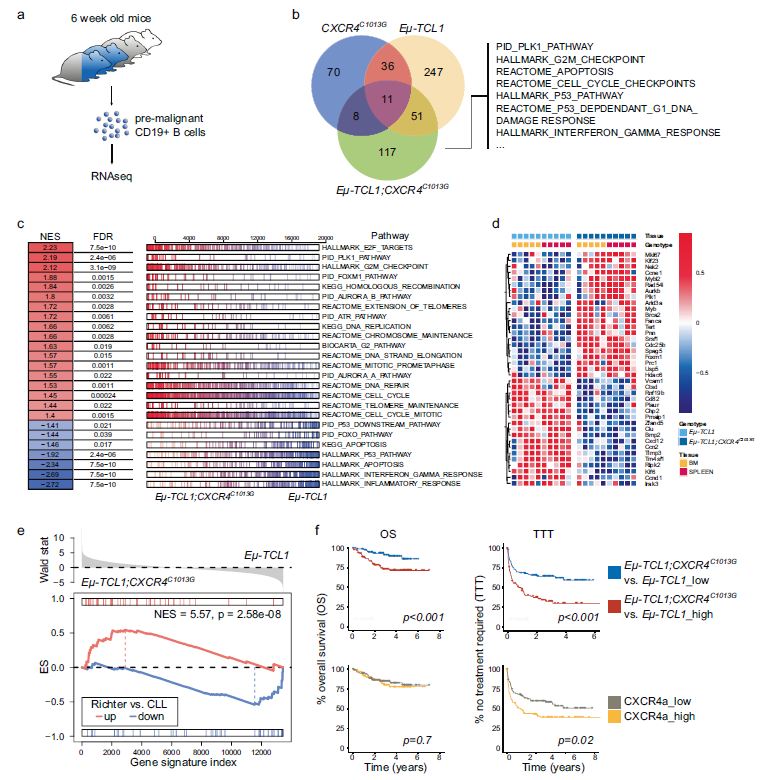
研究人员发现,CXCR4的过度激活会导致过渡型B1淋巴细胞的扩增,其是慢性淋巴细胞白血病(CLL)的前体细胞。在小鼠Eμ-TCL1 CLL模型中,CXCR4的过度激活会导致疾病发作的显著加速并出现更具侵略性的表型。
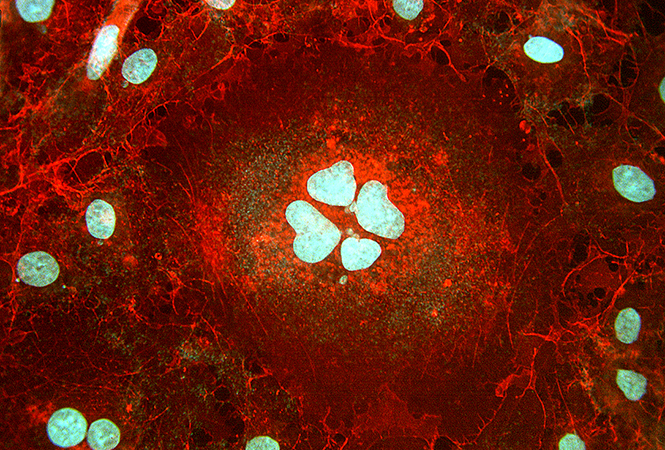
CXCR4过度激活信号的转录特征的鉴定
进一步的研究发现,过度激活的CXCR4信号能够与TCL1协同作用,在B细胞中诱导独特的致癌转录程序,其特征表现为PLK1/FOXM1相关信号通路的激活。相应地,Eμ-TCL1 CXCR4 C1013G B细胞表现出Richter综合征患者相关转录特征的富集,这是CLL的一种侵袭性转化状态。
值得注意的是,在侵袭性淋巴瘤中,MYC的激活与CXCR4的表达水平升高相关。一致的是,在Eμ-Myc小鼠模型(一种侵袭性B细胞癌模型)中,额外的过度激活的CXCR4信号并不影响生存率。
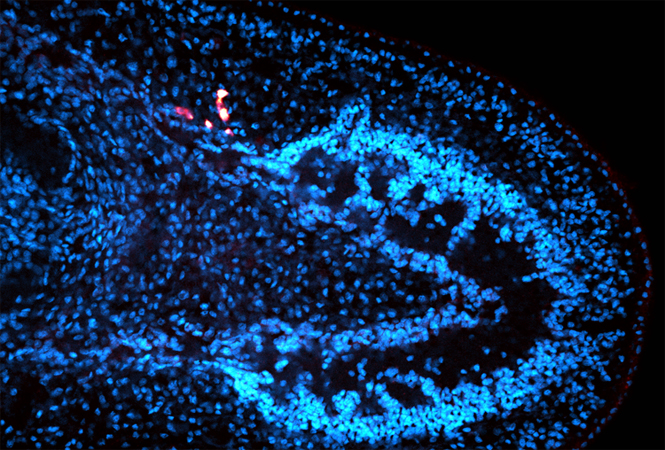
CXCR4和TCL1的共激活介导B细胞中独特的致癌转录程序
总而言之,该研究结果表明,CXCR4的过度激活是侵袭性淋巴瘤表型的一个共同驱动因素。
原始出处:
Lewis, R., Maurer, H.C., Singh, N. et al. CXCR4 hyperactivation cooperates with TCL1 in CLL development and aggressiveness. Leukemia (06 August 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#淋巴细胞白血病#
41
#发生发展#
37
学习了
57
#淋巴细胞#
24
#CXCR4#
51