盘点:胸主动脉疾病研究进展汇总
2016-10-25 MedSci MedSci原创
胸主动脉瘤临床上具有隐匿性,早期检测主要依赖于测定胸主动脉疾病(TAD)临床标志物(二叶主动脉瓣,颅内主动脉瘤,牛型主动脉弓或阳性家族史)。【1】J Am Heart Assoc:单纯性肾囊肿或提示胸主动脉疾病近年来不断有研究报道,单纯性肾囊肿(SRC)与腹主动脉瘤和主动脉夹层相关。为明确SRC是否可作为TAD预测因子,来自耶鲁大学的Ziganshin BA和同事对TAD患者的SRC患病率进行
胸主动脉瘤临床上具有隐匿性,早期检测主要依赖于测定胸主动脉疾病(TAD)临床标志物(二叶主动脉瓣,颅内主动脉瘤,牛型主动脉弓或阳性家族史)。
【1】J Am Heart Assoc:单纯性肾囊肿或提示胸主动脉疾病
近年来不断有研究报道,单纯性肾囊肿(SRC)与腹主动脉瘤和主动脉夹层相关。为明确SRC是否可作为TAD预测因子,来自耶鲁大学的Ziganshin BA和同事对TAD患者的SRC患病率进行了评估。研究结果发表在《J Am Heart Assoc》期刊。
该研究共纳入2004年-2013年间入住耶鲁一纽黑文医院的842名TAD患者(男性64.0%),对照组543名非TAD患者(男性56.2%)。研究者将入组者分为:升主动脉瘤(456,54.2%);降主动脉瘤(86,10.2%);A型主动脉夹层(118,14.0%)和B型主动脉夹层(182,21.6%)4组。采用腹部CT和MRI诊断SRC。
结果发现,升主动脉瘤,降主动脉瘤,A型主动脉夹层和B型主动脉夹层患者的SRC患病率分别为37.5%,57.0%,44.1%和47.3%。对照组SRC患病率为15.3%。虽然整体上男性患者较多(2:1),但主动脉疾病组和对照组SRC患病率并无显著性别差异(1.7:1)。
研究者总结称,“该研究表明TAD患者SRC患病率增加。SRC可作为早期检测TAD风险患者的潜在标志物。”(文章详见--J Am Heart Assoc:单纯性肾囊肿或提示胸主动脉疾病)
【2】Br J Surg:胸主动脉瘤扩张率研究
所有胸主动脉瘤(TAA)患者必须强制性被监测。本研究的目的是,确定TAA的膨胀率和基于TAA直径的监视时间间隔。
纳入有CT扫描形态数据的TAA患者,根据基线TAA直径和达到55 mm理论干预阈值时间,计算年化增长率。基于时间间隔为6 月,1年,2年和3年的模拟成像,发现将达到阈值,但还没有被发现的患者的数量。
995例患者进行了2916次扫描,平均主动脉扩张速率为每年 2.76 mm, 45 mm以上后,呈指数增加。只有3.9%的初始直径为30-39 mm的患者和5.3%的初始直径为40-44 mm的患者,在2 年达到直径阈值。相反,初始直径为50-54 mm的患者,2年扩张到超过55 mm的概率是74.5%,3年概率是85.7%。
基于55 mm的干预阈值,大多数直径低于40 mm的患者可以2年监测一次。45 mm以上患者,建议每年监测。对于直径大于50 mm的患者,可以考虑手术治疗。(文章详见--Br J Surg:胸主动脉瘤扩张率研究)
【3】JACC:单纯性急性主动脉夹层还可选择胸主动脉修复
根据最近的调查结果,胸主动脉修复与单纯性急性主动脉夹层患者的医疗管理有着相似或更好的结果。
中国东南大学中大医院放射科的Yong-Lin Qin博士和同事析338例无并发症的急性B型主动脉夹层患者析338例无并发症的急性B型主动脉夹层患者进行了一项回顾性分析,TEVAR组和医疗管理组分别有184和154人。研究结果包括早期事件(诊断30天内);晚期时间(诊断30天之后);主动脉瓣相关的不良事件,包括破裂、主动脉扩大超过60mm、逆行性A型主动脉夹层、溃疡状突起、内漏和支架诱导新的状况。
数据显示,两组早期事件无显著差异(TEVAR组,10.3%;医疗组,4.5%; P = .064),30天死亡率无差异(TEVAR组,0.5%;医疗组,2.6%;P = .18),不过TEVAR组30天的较轻微的并发症更多,主要是I型内漏 (P < .001)。5年中主动脉相关的不良事件发生率在TEVAR组和医疗组分别为28.2%和37.8%(P = .025);5年全因死亡率分别为10.8%和14.3%(P = .01),主动脉相关的或不明原因的死亡率分别为9.2%和12.1%(P = .012)。晚期事件在医疗组发生率更高(38.3% vs. 23.9%; P = .005),主要是主动脉扩大和破裂。
这项研究证实了TEVAR是这一群患者的可行选择,但TEVAR并没有显著降低早期的死亡率、发病率,TEVAR治疗应该被认为是改善年轻患者晚期预后或更长的寿命预期的选择。(文章详见--JACC:单纯性急性主动脉夹层还可选择胸主动脉修复)
【4】NEJM:胸主动脉瘤致椎体侵蚀-案例报道
男性,74岁,近来出现急性背部疼痛,但不伴有神经系统症状。血压监测结果正常。
据了解,该患者以往有高血压病史,曾因主动脉瘤做过手术和终末期肾功能衰竭行透析。
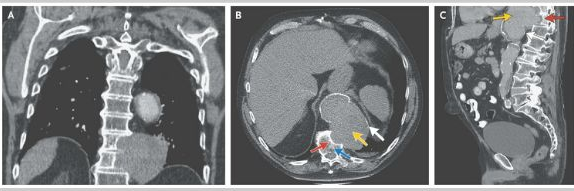
计算机断层扫描结果显示一胸主动脉瘤,测量大小约为8.1cmX11.7cm,病变已侵蚀胸椎T10和T11(图A为冠状切面,图B和图C分别为轴位、矢状面;黄色箭头显示的动脉瘤,红色箭头的是侵蚀部位,蓝色箭头为T11)。
对于胸腰椎的侵蚀,这是主动脉瘤切除术后一种罕见的并发症。通常是因为术后部位因出血导致机械性压迫,从而使病变部位的椎骨相对缺血,使得椎骨破坏。
对于腹膜后肿块诊断,要注意与其他的肿瘤和感染进行鉴别。
由于该患者的一般情况不是很好,因此没有再次行手术进行治疗,而是选择了姑息治疗的方案。3年后,该患者因疾病复发死亡。(文章详见--NEJM:胸主动脉瘤致椎体侵蚀-案例报道)
【5】JACC:非综合征性胸主动脉夹层动脉瘤临床结果预测
该研究旨在比较NS-TAA,MFS和BAV人群的生存和临床结果。
从1988年到2014年进行的一项前瞻性临床研究,患有GA的16-60岁以上的患者被招募。死亡和主动脉夹层危险因素通过Cox比例风险模型确定,并制定了死亡风险评分。
760例患者被诊断为GA(年龄36.9±13.6岁,26.8%为女性; NS-TAA,n=311; MFS,n =221; BAV,n=228)。MFS患者较NS-TAA和BAV年轻。主动脉夹层在NS-TAA比MFS或BAV更为常见。687例患者术后生存>30天,中位随访时间为7年。计算10年死亡率NS-TAA为7.8%,MFS为8.7%,BAV为3.5%(NS-TAA和MFS vs BAV P<0.05)。与全因死亡率有关的因素是MFS(P=0.04),患病时的年龄和夹层的家族史。
MFS和NS-TAA的临床结果相似,但比BAV更糟糕。死亡率的独立预测因子,包括主动脉夹层家族史和年龄,可以包含在一个Aortopathy死亡风险评分中预测生存。NS-TAA管理,包括外科手术,应该与MFS是类似的。(文章详见--JACC:非综合征性胸主动脉夹层动脉瘤临床结果预测)
【6】PLoS One:FBN-1基因的遗传变异与胸主动脉夹层相关
美国耶鲁大学的一项研究表明,FBN-1基因单核苷酸多态性rs2118181与胸主动脉夹层(TAD)具有相关性。论文于4月17日在线发表于 PLoS ONE 。
近期,LeMaire等研究者发现,GWAS研究显示,在FBN-1基因中的两个单核苷酸多态性(rs2118181 和rs10519177)与胸主动脉夹层、胸主动脉瘤(TAA)和胸主动脉瘤或夹层(TAAD)有关。该研究旨在验证上述结果。
此项研究共纳入637例TAAD患者和275例对照组,其中TAD和胸主动脉瘤(TAA)患者分别为140例和497例。确定受试者的rs2118181和rs10519177基因型。对性别、年龄、研究中心和高血压进行校正之后,利用Logistic回归模型评估基因型与TAD、TAA和TAAD的相关性。
结果显示,rs2118181与TAD具有相关性。与未携带者相比,rs2118181携带者的TAD未校正比值比为1.80;对性别、年龄、研究中心和高血压进行校正之后,TAD比值比为1.87。rs2118181风险变异携带者和未携带者在TAD潜在混淆因素主动脉大小方面并无显著差异(平均主动脉大小为5.56和5.48)。rs2118181与TAA和TAAD无相关性。rs10519177与TAD、TAA和TAAD均无相关性。(文章详见--PLoS One:FBN-1基因的遗传变异与胸主动脉夹层相关)
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#疾病研究#
42
#胸主动脉#
29
#主动脉疾病#
29
#研究进展#
23
#主动脉#
29