JACC: CoreValve研究——高危患者TAVR或SAVR术后5年结局竟相似
2018-12-09 国际循环编辑部 国际循环
近日,JACC发表了CoreValve美国核心高风险试验5年随访结果,这是第一项在手术高死亡风险患者中显示,经导管主动脉瓣置换术(TAVR)与外科主动脉瓣置换术(SAVR)相比,具有1年死亡率优势的随机试验。
近日,JACC发表了CoreValve美国核心高风险试验5年随访结果,这是第一项在手术高死亡风险患者中显示,经导管主动脉瓣置换术(TAVR)与外科主动脉瓣置换术(SAVR)相比,具有1年死亡率优势的随机试验。
研究者将TAVR与SAVR进行比较,以获得安全性、性能和耐用性的5年中期结果。将外科高危患者按1:1随机分配至TAVR自膨胀生物瓣膜组或SAVR组。应用VARC-1(Valve Academic Research Consortium I)定义。重度血流动力学结构瓣膜恶化被定义为平均梯度压≥40 mm Hg或梯度≥20 mm Hg的变化或新发重度主动脉瓣关闭不全。计划进行为期5年随访。
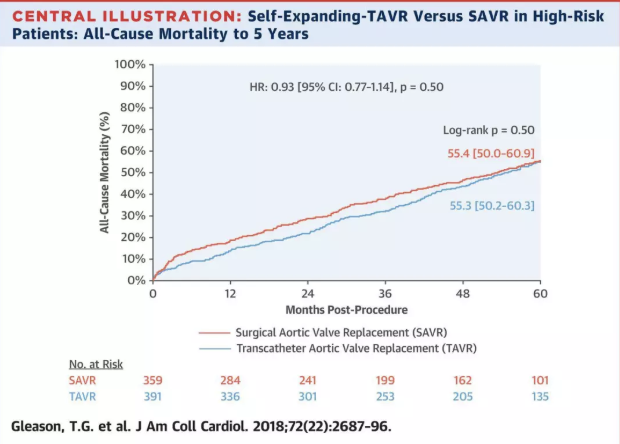
结果显示,共随机纳入美国45个中心的797例患者,其中750例患者尝试进行瓣膜植入(TAVR=391,SAVR=359)。总体平均年龄为83岁,STS评分为7.4%。5年时全因死亡率TAVR组为55.3%,SAVR组为55.4%。亚组分析显示,两组死亡率无显著统计学差异。卒中发病率TAVR组为12.3%,SAVR组为13.2%。平均主动脉瓣梯度压TAVR组为(7.1±3.6)mm Hg,SAVR组为(10.9±5.7)mm Hg。未观察到临床显著瓣膜血栓形成。无重度结构性瓣膜退化(SVD)TAVR组为99.2%和SAVR组为98.3%(P=0.32),无需瓣膜再介入TAVR组为97.0%,SAVR组为98.9%(P=0.04)。5年时,患者永久起搏器植入率TAVR组为33.0%和SAVR组为19.8%。
研究提示,TAVR或SAVR术后高危患者的中期生存率和卒中发生率相似。重度结构性瓣膜恶化和瓣膜再次介入并不常见。
原始出处:
Thomas G. Gleason, Michael J. Reardon, Jeffrey J. Popma, et al. 5-Year Outcomes of Self-Expanding Transcatheter Versus Surgical Aortic Valve Replacement in High-Risk Patients. JACC. Volume 72, Issue 22, December 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CoreValve#
37
#AVR#
25
#JACC#
23
#valve#
32
#高危患者#
34
#ACC#
26
#SAVR#
39
#CORE#
39