Chest:失眠伴随心血管疾病!
2017-02-12 MedSci MedSci原创
失眠是美国最普遍的睡眠障碍,并且常伴随许多心血管疾病。在过去十年中,许多观察性研究已经证明了失眠与心血管疾病(CVD)的发病率和死亡率之间存在着一定的关联性,包括高血压、冠心病和心力衰竭。目前关于两者之间的相关研究存在一些结论的不一致,这可能是由于如何定义和测量失眠的方法不一所致。现有研究数据表明,失眠,特别是伴有短睡眠持续时间,与高血压、冠心病和复发性急性冠状动脉综合征以及心力衰竭的风险增加有关
失眠是美国最普遍的睡眠障碍,并且常伴随许多心血管疾病。
在过去十年中,许多观察性研究已经证明了失眠与心血管疾病(CVD)的发病率和死亡率之间存在着一定的关联性,包括高血压、冠心病和心力衰竭。
目前关于两者之间的相关研究存在一些结论的不一致,这可能是由于如何定义和测量失眠的方法不一所致。
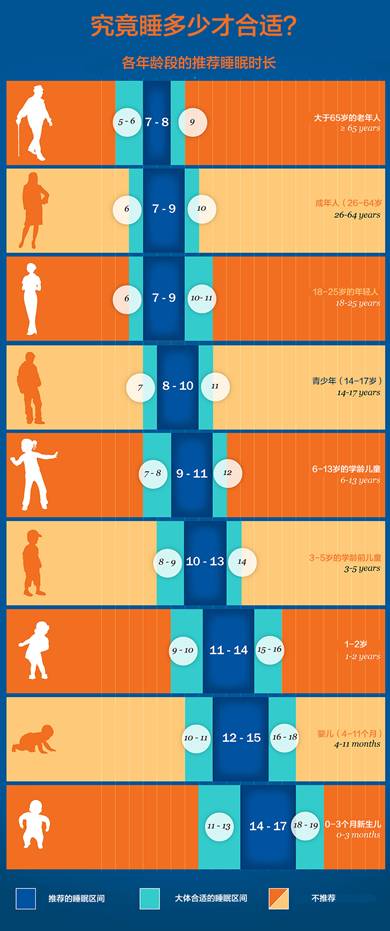
现有研究数据表明,失眠,特别是伴有短睡眠持续时间,与高血压、冠心病和复发性急性冠状动脉综合征以及心力衰竭的风险增加有关。
原始出处:
Javaheri S, Redline S. Insomnia and risk of cardiovascular disease. Chest. 2017 Jan 30. pii: S0012-3692(17)30134-4.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Chest#
22
#EST#
26
#血管疾病#
36
最新研究进展
68
失眠终结
79