Ann Oncol:我国学者展示非小细胞肺癌的精准治疗方案
2017-07-10 转化医学网 转化医学网
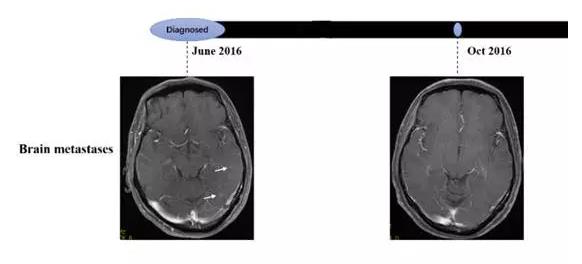
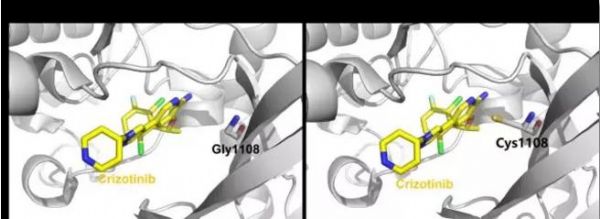
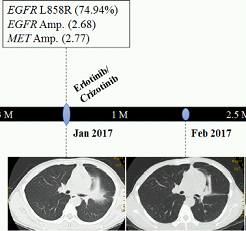
近日,国际经典肿瘤学临床期刊《肿瘤学年鉴》(Annals of Oncology,SCI影响因子11.855)以短文(Letter)的形式发表了广州医科大学第二附属医院李宇清教授联合上海渥恩生物科技有限公司(渥恩医学)在非小细胞肺癌治疗方面的最新研究成果,这也是中国肺癌临床经验在国际肿瘤靶向治疗领域的又一次高质量展示,渥恩医学的循环肿瘤DNA(ctDNA)二代基因测序技术(NGS)亦获得了国际同行

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非小细胞#
36
#我国学者#
31
#治疗方案#
29
#Oncol#
25
不错的文章,值得一读
0
#精准治疗#
0
#精准#
21
不错的文章,值得学习
57
不错的文章不错的文章
35
不错的文章,值得一读
47