JACC:二尖瓣手术后起搏器的植入会增加患者死亡风险
2019-05-21 不详 MedSci原创
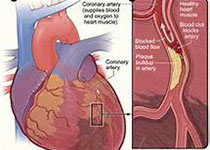
与单独的二尖瓣手术(MVS)相比,MVS伴房颤消融术后的永久性起搏器植入率(PPM)会更高。本研究的目的旨在评估PPM在MVS伴房颤消融术患者中的发生率及临床预后。本研究纳入了243名无PPM植入的房颤患者,随机分成MVS组(n=117)和MVS联合射频消融组(n=126),消融组又随机分为肺静脉分离组(PVI,n=62)和双向迷宫组(n=64),分析结果显示,有35名(14.4%)患者在术后第一
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
28
#二尖瓣手术#
36
#患者死亡#
24
#死亡风险#
34
#起搏器#
46
#ACC#
37
#二尖瓣#
28
#植入#
30