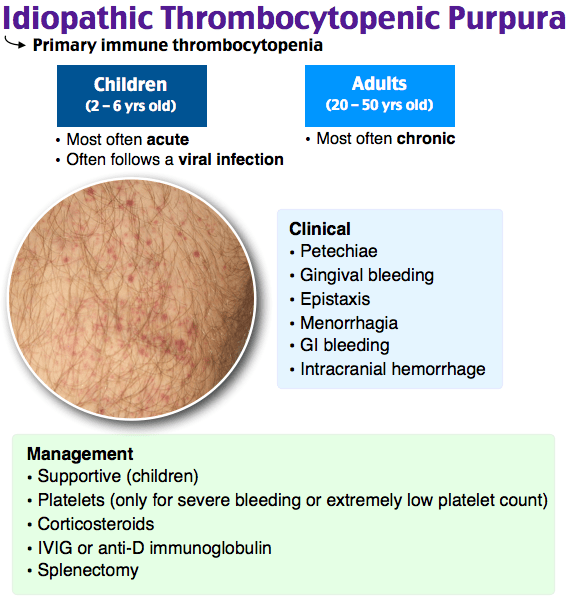
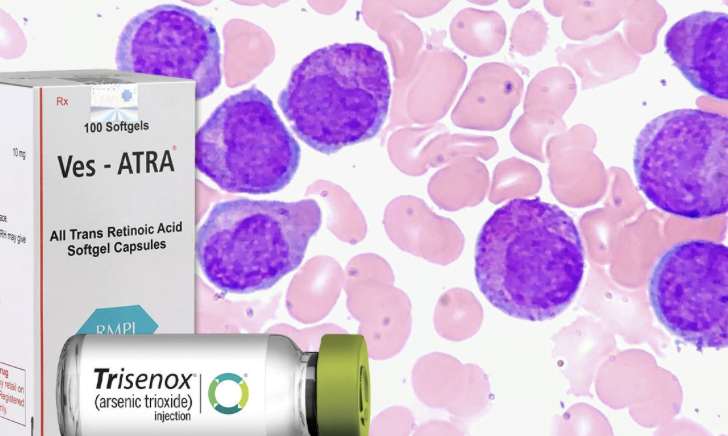
Lancet Haematol:全反式视黄酸加大剂量地塞米松可作为新诊断免疫性血小板减少症患者的一线治疗
2022-01-04 MedSci原创 MedSci原创
全反式维甲酸和大剂量地塞米松的组合在新诊断的原发性免疫性血小板减少症患者中是安全且有效的,提供了持续的反应。该方案代表了这种情况下潜在的一线治疗,但需要进一步研究以验证其有效性和安全性。

大剂量地塞米松是免疫性血小板减少症患者的标准初始治疗,但仍有许多患者复发,仍需要进一步治疗,而全反式视黄酸也已被证明可发挥免疫调节作用并促进血小板生成。最近一项多中心、开放标签、随机、对照、2 期实验刊登在了Lancet Haematol期刊上,旨在评估全反式视黄酸加大剂量地塞米松作为新诊断免疫性血小板减少症患者一线治疗的活性和安全性。
 图1:实验流程图
图1:实验流程图

表1:意向治疗人群的基线和临床特征
该实验在中国六个不同的三级医疗中心进行,符合条件的参与者是成年人(年龄 >18 岁),患有初治、新诊断、原发性免疫性血小板减少症,血小板计数低于 30 × 109 血小板/L 或血小板计数低于 50 × 109 血小板/L 和有临床意义的出血。研究人员随机分配 (1:1) 参与者接受全反式视黄酸(10 毫克,每天口服两次,持续 12 周)加高剂量地塞米松(连续 4 天静脉注射 40 毫克/天)或单独使用高剂量地塞米松。如果患者在第 14 天没有反应,则重复 4 天的地塞米松疗程。主要终点是 6 个月的持续反应,定义为血小板计数维持在每升至少 30 × 109 个血小板,并且至少高于基线计数的 2 倍,并且没有出血,此时不需要急救药物。通过意向治疗分析主要终点,并在所有接受至少一剂研究药物的参与者中评估安全性。该试验已在 ClinicalTrials.gov 注册,NCT04217148,现已完成。
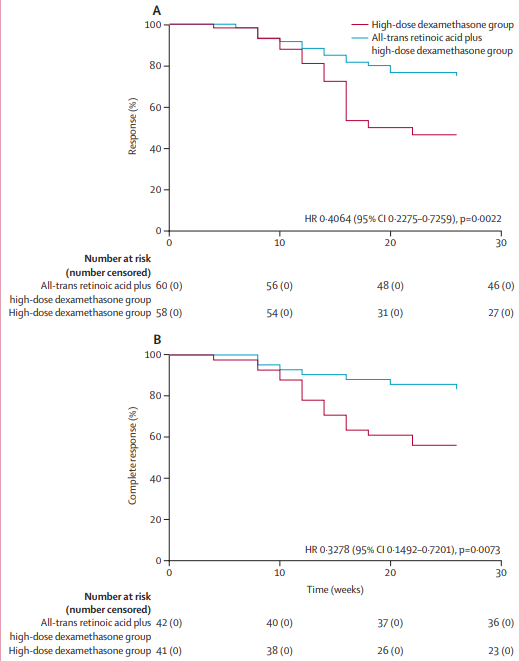
图2:有初始反应的(A)患者和有初始完全反应的(B)。患者的反应持续时间(复发时间)反应持续时间(或复发时间)复发的定义为血小板计数低于每L30×10⁹血小板,血小板计数低于基线计数的2倍,或反应后出血。
在 2020 年 1 月 1 日至 2020 年 6 月 30 日之间,132 名患者被随机分配到全反式维甲酸加高剂量地塞米松(n=66)或单独高剂量地塞米松(n=66)。三名患者没有接受分配的治疗,安全性分析集中剩下 129 名。6 个月时,全反式维甲酸加高剂量地塞米松组(66 人中的 45 [68%])的参与者比例明显高于高剂量地塞米松单药治疗组(66 人中的 27 [41%])有持续的反应(OR 3·095,95% CI 1·516-6·318;p=0·0017)。联合组最常见的不良事件是皮肤干燥(64 名患者中的 31 [48%])、头痛(12 [19%])和失眠(12 [19%]),以及失眠(10 [15%]) 65 名患者)和焦虑或情绪障碍(8 名 [12%])在单药治疗组。两种治疗均耐受良好,未发生 4 级或更严重的不良事件。没有与治疗相关的死亡。
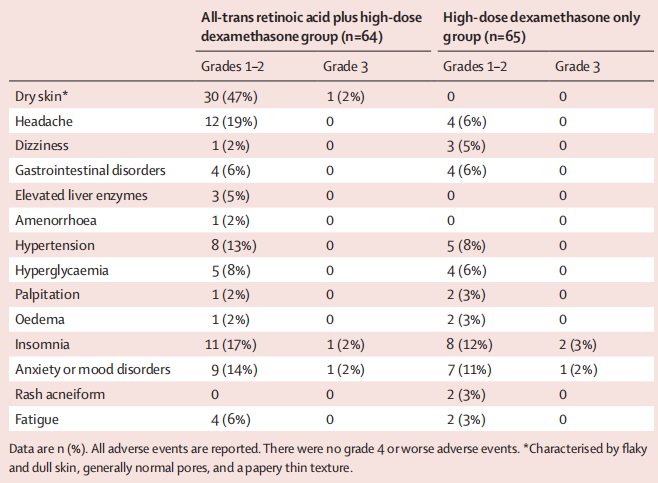
表2:安全分析集中的不良事件
总的来说,研究表明了全反式维甲酸和大剂量地塞米松的组合在新诊断的原发性免疫性血小板减少症患者中是安全且有效的,提供了持续的反应。该方案代表了这种情况下潜在的一线治疗,但需要进一步研究以验证其有效性和安全性。
原始出处:
Huang QS, Liu Y, Wang JB, Peng J, Hou M, Liu H, Feng R, Wang JW, Xu LP, Wang Y, Huang XJ, Zhang XH. All-trans retinoic acid plus high-dose dexamethasone as first-line treatment for patients with newly diagnosed immune thrombocytopenia: a multicentre, open-label, randomised, controlled, phase 2 trial. Lancet Haematol. 2021 Oct;8(10):e688-e699. doi: 10.1016/S2352-3026(21)00240-4. PMID: 34560012.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#HAE#
48
#新诊断#
45
#全反式视黄酸#
36
#Lancet#
36
#免疫性血小板减少#
38
#血小板减少#
58
#EMA#
37
#大剂量#
39
防治及用药的高度重视,HIV双药单一片剂
64