J Clin Lipidol:他汀联合依折麦布 消除动脉粥样斑块更高效
2018-11-20 林巧楠 环球医学
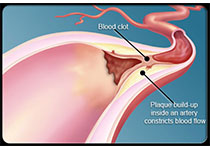
动脉粥样硬化性冠状动脉疾病(CAD),仍然是备受世界关注的引发死亡的常见原因。研究表明,某些风险因素加速了动脉粥样硬化的进展,其中高胆固醇血症越来越受到人们的重视。包括Mendelian随机研究在内的大量证据证明,低密度脂蛋白胆固醇(LDL-C)与CAD的发生存在因果关系。
当前指南建议,高风险心血管疾病患者应通过接受强化降脂治疗使LDL-C达标。他汀类通过抑制HMG-CoA还原酶,使胆固醇合成受阻,而有效降低胆固醇,特别是LDL-C浓度,延缓动脉粥样硬化斑块的形成,临床应用十分广泛。依折麦布是第一个也是目前唯一批准上市的胆固醇吸收抑制剂。既往研究表明,依折麦布联合他汀治疗,或能促进前述患者斑块发生有益变化,然而该作用的报道不一致。
2018年,发表在《J Clin Lipidol》的一项系统评价和Meta分析,考查了依折麦布+他汀vs仅他汀治疗,对血管内超声评估的冠状动脉斑块体积的影响。
8项研究用于制作系统评价,其中共6项研究,包含583名受试者满足Meta分析标准。
结果显示,自基线到随访期总粥样硬化斑块体积显着缩小,MD为-3.71mm3(P<0.001)。然而,粥样硬化斑块体积百分比分析证实加权MD为-0.77%(P=0.10)。观察到LDL-C出现大幅降低,MD为-16.75mg/dL(P<0.00001)。
作者认为,依折麦布联合他汀治疗,可有效缩小血管内超声评估的总粥样硬化斑块体积,也能有效降低血浆LDL-C水平。
据悉,他汀类药物随着剂量增大,降脂作用增加,但不良反应也会增多。依折麦布联合他汀治疗,为不能耐受大剂量他汀患者提供新选择。
近年来,先后完成的以我国及其他亚洲人群为基础的降脂药相关研究表明,大剂量他汀治疗并不能带来更多获益。而上述研究表明,依折麦布联合他汀治疗,不仅能有效缩小血管内超声评估的总粥样硬化斑块体积,也能有效降低血浆LDL-C水平,在此背景下,联合用药或是一种合情合理的新选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉粥样斑块#
42
#IDO#
56
#粥样斑块#
34
#Lipid#
41
#斑块#
39
#依折麦布#
45
学习了学习了
53