J Clin Oncol:III期| 派姆单抗联合伊匹单抗治疗PD-L1 TPS≥50%转移性NSCLC(KEYNOTE-598)
2021-02-01 MedSci原创 MedSci原创
派姆单抗治疗中加入伊匹单抗是否可进一步提高有程序性死亡配体1 (PD-L1)肿瘤比例评分(TPS)≥50%、无可操作的驱动基因突变的转移性非小细胞肺癌患者的治疗效果?
派姆单抗单药治疗是有程序性死亡配体1 (PD-L1)肿瘤比例评分(TPS)≥50%、无可操作的驱动基因突变的转移性非小细胞肺癌(NSCLC)的标准一线治疗。目前尚不清楚,在派姆单抗治疗中加入伊匹单抗是否可进一步提高该类患者的治疗效果。
本研究是一项随机、双盲的III期试验(KEYNOTE-598),招募了既往未治疗过的PD-L1 TPS≥50%且不携带敏感性EGFR或ALK变异的转移性NSCLC患者,随机(1:1)分至伊匹单抗(1 mg/kg·6周x18次)或安慰剂组;所有患者每3周接受一次派姆单抗(200 mg),共35剂。主要终点是总存活期和无进展存活期。
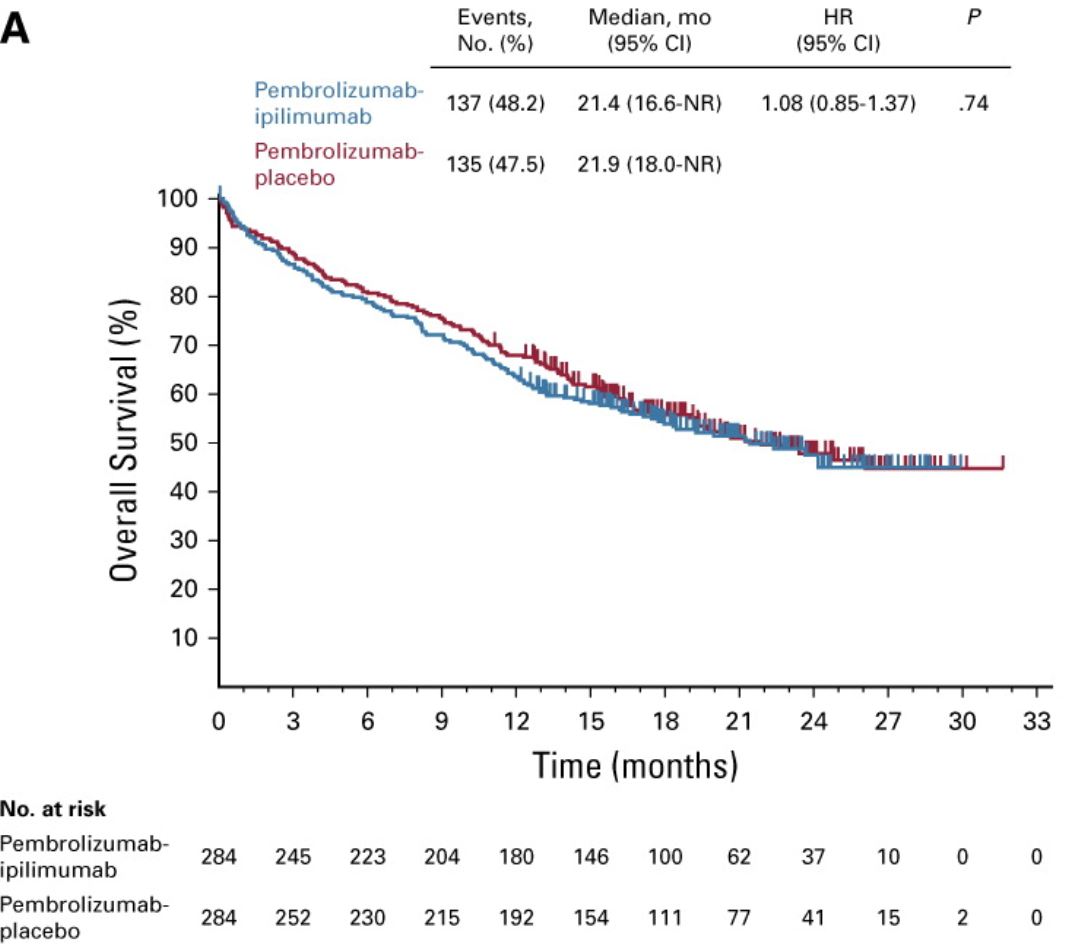
OS
共招募了568位患者,每组各284人。派姆单抗-伊匹单抗组和派姆单抗-安慰剂组的中位总存活期分别为21.4个月和21.9个月(HR 1.08,95% CI 0.85-1.37,p=0.74);中位无进展存活期分别为8.2个月和8.4个月(HR 1.06,95% CI 0.86-1.30,p=0.72)。
PFS
伊匹单抗组和安慰剂组3-5级不良反应发生率分别为62.4%和50.2%,死亡率分别为13.1%和7.5%。外部数据和安全监测委员会建议停止这项无效研究,受试者停用伊匹单抗和安慰剂。
综上,派姆单抗治疗加入伊匹单抗并不能在派姆单抗单药疗法的基础上进一步提高PD-L1 TPS≥50%、无可靶向的EGFR或ALK变异的转移性NSCLC患者的治疗效果。因此,该研究不支持该类患者采用派姆单抗联合伊匹单抗治疗。
原始出处:
Michael Boyer, et al. Pembrolizumab Plus Ipilimumab or Placebo for Metastatic Non–Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score ≥ 50%: Randomized, Double-Blind Phase III KEYNOTE-598 Study. Journal of Clinical Oncology. January 29, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
70
#转移性NSCLC#
41
#III#
37
#KEYNOTE#
51
#派姆单抗#
42
#PD-L1#
42
#转移性#
40
#III期#
30
学习赚积分
94
肿瘤免疫是大家关心的话题,K药与其它药对比,值得关注!
64