PNAS:人脑脊液中的朊蛋白定量——助力朊病毒病药物开发
2019-04-03 海北 MedSci原创
降低脑中的天然朊蛋白(PrP)水平是治疗或预防人朊病毒病的有吸引力的策略。任何PrP降低治疗剂的临床开发将需要适当的药效学生物标志物:用于量化PrP的实用且稳健的方法,并且可靠地证明其在活体患者的中枢神经系统(CNS)中的减少。
降低脑中的天然朊蛋白(PrP)水平是治疗或预防人朊病毒病的有吸引力的策略。任何PrP降低治疗剂的临床开发将需要适当的药效学生物标志物:用于量化PrP的实用且稳健的方法,并且可靠地证明其在活体患者的中枢神经系统(CNS)中的减少。
最近,研究人员评估了基于ELISA的人类脑脊液(CSF)中人类PrP定量的潜力,作为PrP减少治疗的生物标志物。
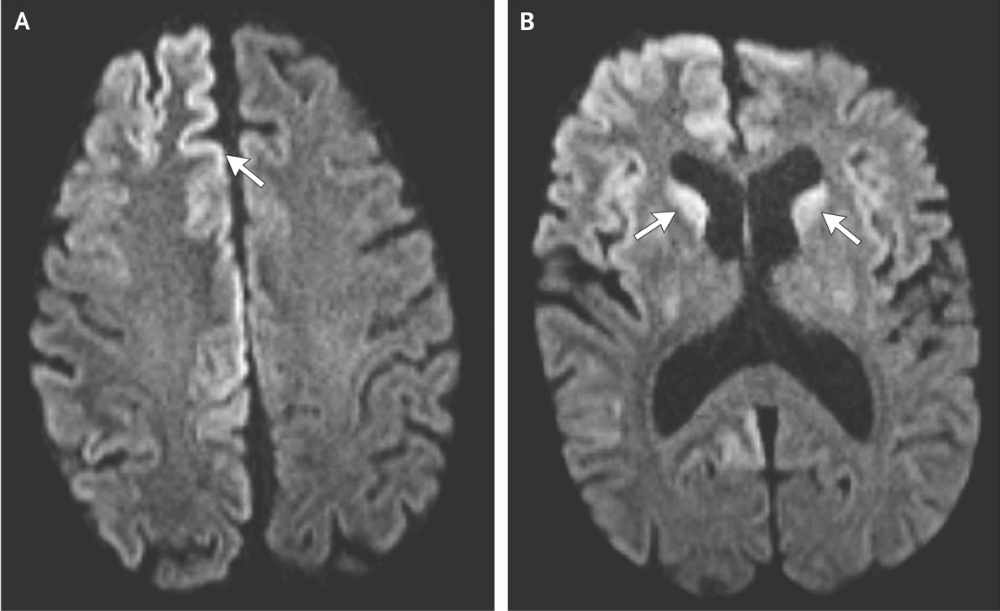
研究人员表明,CSF PrP在处理和储存过程中对塑料吸附非常敏感,但通过添加洗涤剂可以使其损失最小化。研究人员发现,血液污染不影响CSF PrP水平,并且CSF PrP和血红蛋白是不相关的,这一起表明CSF PrP是CNS衍生的,支持其监测感兴趣组织的相关性,并且与脑中相对于血液高的PrP丰度保持一致。
在具有受控样本处理的队列中,CSF PrP表现出良好的受试者内重测信度(平均变异系数,相隔8-11周收集的样本中的13%),足够稳定的基线以允许治疗上有意义的脑PrP减少的检测。
总之,这些发现提供了一种监测PrP降低药物在CNS中的作用的方法,并且将利用这种作用机制促进朊病毒病治疗剂的开发。
原始出处:
Vallabh SM et al. Prion protein quantification in human cerebrospinal fluid as a tool for prion disease drug development. PNAS, 2019; doi: 10.1073/pnas.1901947116.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PNAS#
42
#朊蛋白#
37
mark
65
#药物开发#
48
向挑战病魔的科研人员致敬!
67