Laryngoscope:人工耳蜗植入后的听力变化评估
2022-01-03 AlexYang MedSci原创
调查了人工耳蜗(CI)植入者的听力随时间变化情况,确定了基于设备类型和人口统计学因素的听力结果差异,还确定了CI后早期听力损失的程度与随后的听力损失率之间是否有关系。
过去20年,人工耳蜗(CI)技术和设计的进步,以及临床实践和手术技术的进步,使得CI候选者的范围得以扩大。尽管取得了这些进展,CI之后保留有用的声学听力仍然是一个挑战,许多研究报告称在植入后的几周至几个月内,听力水平与术前相比会下降,且导致这种听力损失的机制仍然未知。

近期,来自美国的研究人员再《Laryngoscope》上发表文章,调查了人工耳蜗(CI)植入者的听力随时间变化情况,确定了基于设备类型和人口统计学因素的听力结果差异,还确定了CI后早期听力损失的程度与随后的听力损失率之间是否有关系。
研究为前瞻性、单一对象研究。研究包括了211名接受听力保护性CI的受试者:80名接受Nucleus Hybrid L24(Cochlear),47名接受422/522(Cochlear),24名接受S8(Cochlear),14名接受S12(Cochlear),6名接受SRW(Cochlear),21名接受SLIM J(Advanced Bionics),以及19名接受Flex(Med-EL)。其中有127人纳入后续分析。研究人员收集并比较了术前和术后的听觉阈值(低频纯音平均数)。
研究结果发现,L24的长期听力保存率为65%(52/80),S8为83%(20/24),S12为79%(11/14),SRW为83%(5/6),422/522为54%(25/47),SLIM J为91%(21/23),Flex为84%(16/19)。听力损失与设备类型(P=0.9105)或性别(P=0.2169)没有关系。在设备激活后,老年受试者(年龄≥65岁)的听力结果比年轻受试者(年龄<65岁,P=0.0262)更差。随着时间的推移,老年患者和年轻患者的听力损失率没有明显差异(P=0.0938)。最初的术后听力损失与长期听力损失率也没有关系。
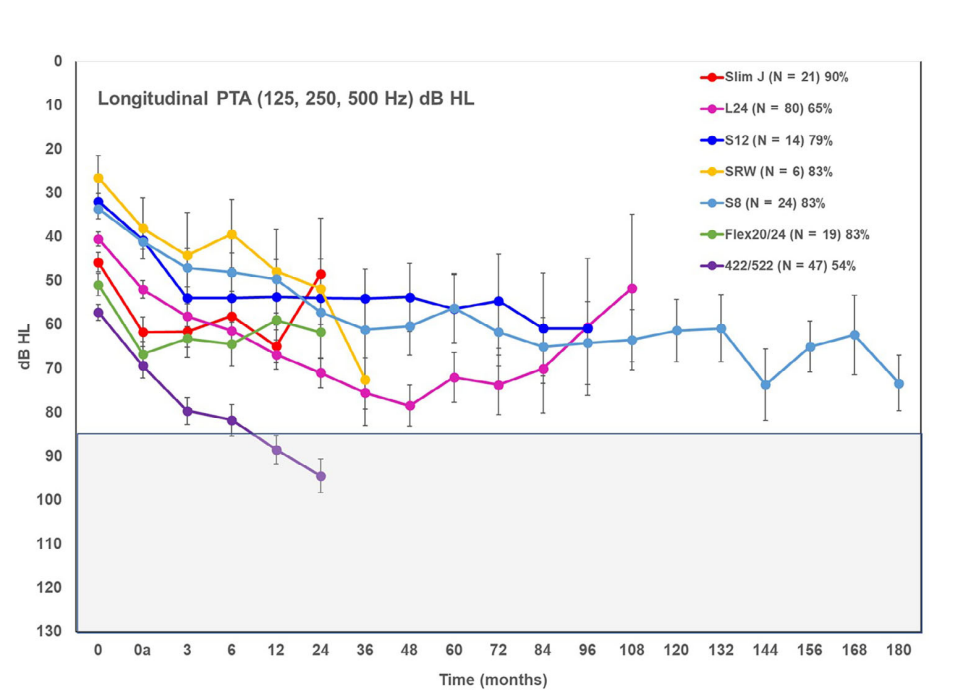
长期的听力结果情况(低频125-500Hz PTAs)
综上所述,CI受试者有可能长期保持低频听力,并且与性别或设备类型无关。随着时间的推移,听力损失率不取决于患者的年龄。CI后的早期听力损失也并不能预测长期的听力损失率。
原始出处:
Megan J Jensen , Heba Isaac , Helin Hernandez et al. Timing of Acoustic Hearing Changes After Cochlear Implantation. Laryngoscope. Dec 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#PE#
38
评论
0
#听力#
52
#人工耳蜗#
47
#植入#
37
#耳蜗植入#
30