BMJ: 我国17%急性心梗患者仍使在用硫酸镁!China PEACE研究全新分析
2020-03-31 中国循环杂志 中国循环杂志
1991年公布的ISIS-4大规模临床试验结果推翻既往认知,提出静脉镁剂不仅对降低急性心肌梗死无益,甚至有害。自2000年起,国内外指南均不主张在急性心肌梗死患者中常规使用静脉镁。
1991年公布的ISIS-4大规模临床试验结果推翻既往认知,提出静脉镁剂不仅对降低急性心肌梗死无益,甚至有害。自2000年起,国内外指南均不主张在急性心肌梗死患者中常规使用静脉镁。
近期,阜外医院学者王现强、杜雪等在BMJ Open发表的China PEACE研究最新分析显示,虽然静脉硫酸镁的使用有所下降,但直到2015年,每6例急性心肌梗死患者中仍有1人接受这种治疗。
研究显示,15年来,我国急性心肌梗死患者中静脉硫酸镁的总体使用率已从2001年的32.1%降至2015年的17.1%,而且这一变化主要发生在前5年间。
与中部地区(25.9%降至18.1%)相比,东部(33.3%降至16.5%)和西部(34.8%降至17.2%)地区的下降幅度更大,但城乡之间无明显差异。
值得关注的是,使用静脉硫酸镁的医院比例在既往15年却无明显变化(81.3%至77.9%)。
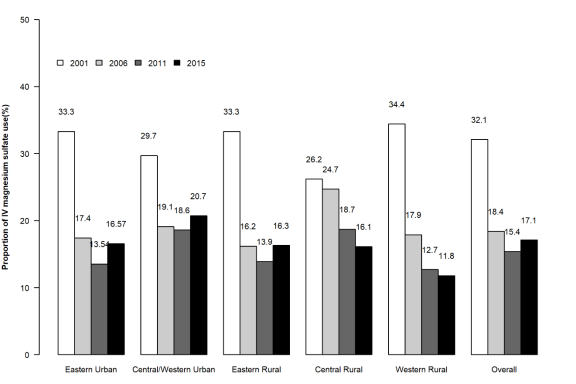
图1 2001年、2006年、2011年和2015年5个经济/地理地区的静脉硫酸镁使用率的变化趋势
研究还提示,静脉硫酸镁的使用与入院时心脏骤停,再灌注治疗以及院内新发心力衰竭显著相关。
此外,接受静脉硫酸镁治疗的患者出现院内死亡及院内并发症的风险更高。
研究者认为,从静脉硫酸镁使用来看,我国急性心肌梗死的诊疗模式改善还存在较大差距,特别是近10年间,总体使用率仍在高位徘徊。
当前我国医疗质量控制工作的关注重点多为“该用的药是否使用”,然而对于“不该用药是否弃用”仍缺乏持续的评估。
研究者强调,鉴于此,除了加强针对医务人员的指南培训和知识更新,还需要不断健全医疗质量评价体系,以推进持续改善患者预后并减少资源浪费。
这项China PEACE研究最新分析,于分层随机抽样入选的162家医院中,通过回顾性注册登记研究对其急性心肌梗死的诊疗模式进行了为期15年(2001~2015)的随访,共纳入24418例排除低镁血症或尖端扭转室性心动过速等硫酸镁适应证的急性心肌梗死患者。
原始出处:
Wang X, Du X, Yang H, et al. Use of intravenous magnesium sulfate among patients with acute myocardial infarction in China from 2001 to 2015: China PEACE-Retrospective AMI Study. BMJ Open, 2020, 10(3): e033269.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CHINA#
38
#PE#
32
#心梗患者#
38
#ACE#
35
#BMJ#
30
#急性心梗#
52
#硫酸镁#
35