Cell研究探讨癌细胞的“喷射器”
2017-03-01 张迪 生物通
有时细胞会为了抵抗药物治疗而将药物“吐出来”,尤其是癌细胞,当进行细胞致死性的化疗治疗时,癌细胞就会做出如此举动。近期来自洛克菲勒大学的研究人员解析了这种“分子泵”的原子水平三维结构,深入探讨它的作用机制。
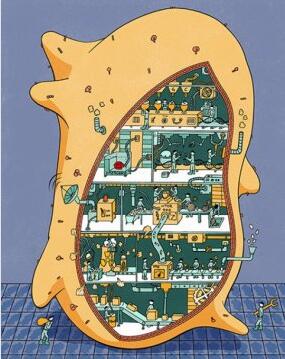
这一研究成果在线公布于2月26日的Cell杂志上,文章的通讯作者是洛克菲勒大学陈珏(Jue Chen,音译)研究员,她的研究组主要聚焦于一类被称为ATP结合盒转运体(ATP-binding cassette,ABC transporters)蛋白。对于最新这项研究,她表示,“这种分子机器能喷射出许多抗癌剂以及其它药物,但是至今大家都不是很清楚为何这种喷射器能识别和喷射出多种物质。”
“我们通过分析这种耐药性‘分子泵’在转运之前如何与其‘货品’结合,从而找到了一个答案,”她补充说。这一新的结构将有助于指导更有效的癌症治疗方法,也能用于其它疾病的治疗。
神秘的多功能
多药耐药相关蛋白1(multidrug resistanec-associated protein1,MRP1)最早是于1992年在耐药性肺癌细胞中被鉴定出来,虽然一些癌细胞中,这种蛋白表达丰度异常高,但是它在正常细胞内也很常见。MRP1可以作为保护大脑免受感染屏障的部分组成元件,也可以帮助分泌激素,传递免疫信号化合物,以及运输其它等“货品”,如有害的外来物质。而且对于现代医学,MRP1并不是一个有益的因子,因为它会经常错误运输有用的化学品,包括阿片剂,抗抑郁药和抗生素,这对于需要去除这些物质的治疗来说具有潜在害处。
MRP由MRP1-9共9个成员组成,与其它药物转运蛋白一样,都是需要挑选转运的“货品”,之前的研究表明MRP1参与了某些肿瘤的耐药作用,被认为是介导肿瘤多药耐药的主要跨膜转运蛋白之一,探讨MRP1的结构、功能,以及与肿瘤的关系,有利于指导临床合理用药和肿瘤预后的评估。但是目前研究人员无法详细了解这种蛋白,因为研究分子结构的标准方法需要将分子转变成晶体,但MRP1无法得到晶体结构。
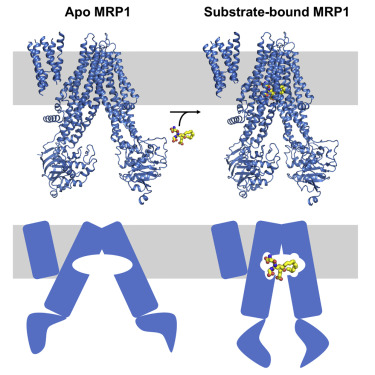
陈珏研究组的博士后Zachary Johnson利用冷冻电镜技术解决了这个问题,在这种技术中分子被冷冻在溶液中,而不是晶体中,这样他们捕获到了MRP1的单独结构,以及其与“货品”结合的结构。
两部分组成的口袋
研究人员深入探索了MRP1内部结构,他们发现这个蛋白的多能性奥秘:MRP1与其“货品”结合的口袋结构。这个结构是由泵的两侧组成,结构十分灵活,能容纳不同尺寸的分子。而且口袋有两个部分,每个部分都有不同的化学特性,研究表明许多结合上MRP1的底物都与口袋的两部分结构匹配。
“货品”一旦进入口袋,就会与MRP1两部分相连接,将它们拉在一起,就像是夹核桃夹子的两只脚,这是改变泵形状的第一步,之后蛋白就能将“货品”运送到细胞外部。
MRP1是参与整个身体许多生理过程的运算蛋白家族的一部分,家族其它成员也能喷射药物,因此这项工作具有除了解析MRP1以外的更多医学意义。
“最终我们希望这种类似结构能作为泵无法识别的化疗药物设计模版,或者研发阻断这些结构的抑制剂。这种方法可能也可以用于提高其它药物的药效,例如那些需要送达到大脑中的药物。”
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
25
学习了,谢谢分享!
61
最新研究探讨癌细胞的喷射器。
58
最新研究探讨癌细胞。
71
#CEL#
0
#癌细胞#
0