NEJM:对NSCLC患者使用nivolumab和docetaxel药物之间的区别
2015-07-10 MedSci MedSci原创
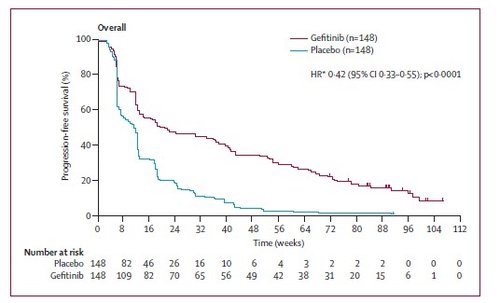
背景:处于晚期的鳞状非小细胞肺癌(NSCLC)患者病情恶化或一期化疗后可供选择的治疗方案非常有限。这项随机、开放、国际化的三期研究方案目的在于评估nivolumab这一药物的安全性和有效性,并比较nivolumab药物和多西他赛药物治疗患者后患者生存率的区别。方式:我们随机选取272名患者,将其随机分为两组,一组接受nivolumab药物治疗,剂量为每两周3mg/kg,另一组患者接受多西他赛药物治
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
23
#SCLC患者#
24
#NIV#
30
请问有全文吗?
21
看看
105
#NSCLC患者#
0
看看
63