JACC:经皮除颤器植入的安全性和疗效性研究
2017-08-10 MedSci MedSci原创
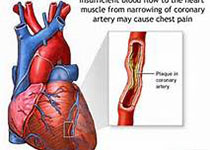
经皮电复律除颤器的植入(S-ICD)是用来治疗室性心律失常的技术,S-ICD临床结果和成本效益因素评价(EFFORTLESS S-ICD)的数据库记录了985名患者5年的随访预后情况。近日,在国际心血管权威杂志JACC上发表了一篇旨在通过EFFORTLESS S-ICD数据库评估分析S-ICD的安全性和不良休克发生率的临床研究。本研究的主要终点事件是术后30天和360天的并发症,心房颤动或室上性心
经皮电复律除颤器的植入(S-ICD)是用来治疗室性心律失常的技术,S-ICD临床结果和成本效益因素评价(EFFORTLESS S-ICD)的数据库记录了985名患者5年的随访预后情况。近日,在国际心血管权威杂志JACC上发表了一篇旨在通过EFFORTLESS S-ICD数据库评估分析S-ICD的安全性和不良休克发生率的临床研究。本研究的主要终点事件是术后30天和360天的并发症,心房颤动或室上性心动过速所致的休克。队列的平均随访时间是3.1 ± 1.5年,有82名患者完成了完整的5年随访调查,患者的平均年龄是48岁,女性占28%,左室射血分数为43 ± 18%,65%的患者建议首次接受介入治疗。研究结果显示,S-ICD的手术并发症在30天和360天分别是4.1%和8.4%。少数患者由于心动过速(n=5)、双心室起搏(n=4)或心动过缓(n=1)而需要将植入设备取出。休克的发生率在1年和3.1年的分别是8.1%和11.7%。在植入的患者中,99.5%取得了理想的疗效。研究结果表明,经皮电复律除颤器的植入的安全性和有效性是值得肯定的。原始出处:Lucas B et al.Implant a
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
25
#ACC#
26
#除颤#
34
#植入#
23
研究设计有创新性
70
方便快捷恢复快
68