JACC:人类首例经导管大血管吻合术!
2017-08-05 MedSci MedSci原创
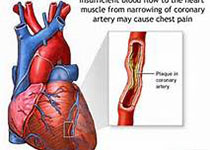
目前,对于先天性心脏病的治疗,经导管介入治疗已经代替了许多外科治疗,比如房间隔缺损修补。但是,一些复杂的先心病仍然需要外科的开胸手术治疗,有些甚至需要多期的开胸外科治疗,这就不可避免地伴随着较高的死亡率。近日,在国际心血管权威杂志JACC上发表了一篇旨在评估在一个病人中仅经导管操作行大血管吻合术(上腔静脉和肺动脉吻合术)的可行性的临床研究。 研究者在近十年一直在探索非外科方法的大血管吻合方法
目前,对于先天性心脏病的治疗,经导管介入治疗已经代替了许多外科治疗,比如房间隔缺损修补。但是,一些复杂的先心病仍然需要外科的开胸手术治疗,有些甚至需要多期的开胸外科治疗,这就不可避免地伴随着较高的死亡率。近日,在国际心血管权威杂志JACC上发表了一篇旨在评估在一个病人中仅经导管操作行大血管吻合术(上腔静脉和肺动脉吻合术)的可行性的临床研究。
研究者在近十年一直在探索非外科方法的大血管吻合方法和技术。在本研究中,研究者拟对一名成年伴有严重青紫的先心病患者行经导管上腔静脉和肺动脉吻合术,并在术前根据患者的3D心脏模型进行了体外模拟实验。本研究是人类首次仅经导管行上腔静脉肺动脉吻合术,该患者是名35岁的成年女性,因呼吸困难和青紫,被诊断为功能性单心室,伴有少量的肺血流。心脏外科专家认为根据患者的全身情况,外科手术的风险会较大。经导管吻合术后,患者恢复良好,并在术后6个月,临床症状有明显的改善。
经导管上腔静脉肺动脉吻合术在治疗单心室等复杂先心病上是可行的,可以为复杂先心患者提供了另一种治疗途径。
原始出处:
Kanishka R et al.First-in-Human Closed-Chest Transcatheter Superior Cavopulmonary Anastomosis.JACC.2017 Aug.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#吻合术#
31
#JACC#
19
#大血管#
31
厉害
53
技术真先进,认真学习
57
#ACC#
33
#经导管#
0
学习,谢谢分享
59
学习了谢谢分享
72
值得推荐一下
59