小知识:重症患者循环保护通气策略
2016-07-23 中华内科杂志 中华内科杂志
mlwdGlvbiByZGY6YWJvdXQ9IiIgeG1sbnM6eG1wPSJodHRwOi8vbnMuYWRvYmUuY29tL3hhcC8xLjAvIiB4bWxuczp4bXBNTT0iaHR0cDovL25zLmFkb2JlLmNvbS94YXAvMS4wL21tLyIgeG1sbnM6c3RSZWY9Imh0dHA6Ly9ucy5hZG9iZS5jb20veGFwLzEuMC9zV
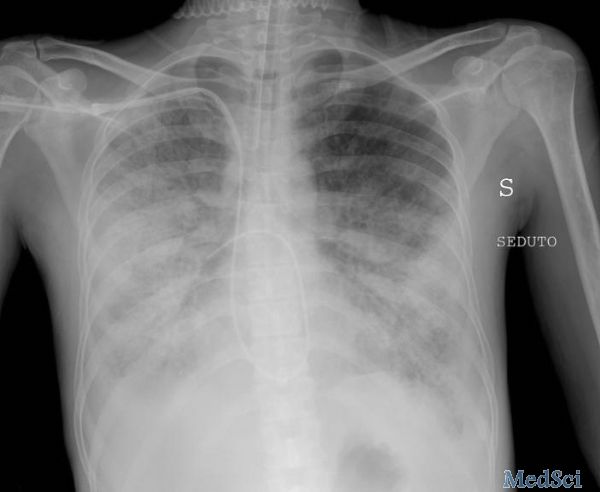
当一个重症病人同时需要液体复苏、血管活性药物、机械通气等治疗时,我们常常需要考虑机体的所有器官,尤其是心肺,患者可能需要积极容量复苏,但也要顾及心脏的承受能力,患者可能需要使用较大的PEEP才能维持基本氧合水平,同时也要稳住血压不要崩塌。对于ARDS患者而言更是如此,肺保护策略已是常规,但越来越多研究表明ARDS患者最终并非死于严重肺损伤或顽固性低氧血症,而是死于休克和突发心跳骤停。
在当前的机械通气策略中仅仅强调肺保护可能还不足,更应该关注呼吸运动产生的血流动力学效应,在开放肺、保护肺的同时应避免机械通气对循环的损伤,进而达到改善患者预后的目的。
临床上可能很多人都在有意无意做着“保护循环性机械通气”的工作,但像刘大为教授这样白纸黑字提出来的应该还是首次。
一、机械通气对血流动力学的影响及循环保护性策略的提出
气道高压导致循环回心血量不足:正压通气在扩张气道、肺泡的同时,增加胸腔内压,影响静脉回流,这是最基本的常识。当患者顽固性低氧时,我们可能会采用较高的PEEP,而PEEP也会引起上下腔静脉回流阻力升高,导致回心血量减少。
正压机械通气对左、右心的影响:ARDS时可导致肺血管顺应性下降,增加右心后负荷,甚至可以出现急性肺动脉高压、右心功能障碍。而使用肺复张及高PEEP在复张塌陷肺泡的同时,导致相对正常区域的肺泡过度膨胀,也会增加右心负荷、降低心输出量及恶化血流动力学等。而机械通气对左心的影响较为复杂,起初由于减少回心血量、减轻左心后负荷有助于心脏射血,但由于右心的影响(如上述)最终导致左心前负荷不足、左心搏出量减少、体循环低血压。
ARDS本身即存在血流动力学紊乱,而机械通气策略又可能加重血流动力学紊乱,这种机械通气与循环之间的关系已日益被人重视,调节好心肺相互关系已经成为重症医师的巨大挑战。正因为如此,刘大为教授的团队提出:“在机械通气时,实施以血流动力学评估和血流动力学治疗为导向的循环保护性通气策略,旨在强调实施机械通气时保护循环功能和维持血流动力学稳定,以进一步改善患者预后。”
在提出这个策略之前,我们临床医师肯定或多或少关注机械通气与血流动力学之间的关系,刘大为教授这样白纸黑字的提出,对于我们临床工作的指导有帮助。
二、如何实施循环保护性通气策略?
光提出策略是不够的,还得有具体的实施方法。在机械通气过程中,任何机械通气条件的改变都可能对血流动力学造成影响,比如潮气量、呼吸频率、PEEP等。为避免通气设置对血流动力学的不利影响,应在机械通气前进行血流动力学评估,并以血流动力学治疗为导向调整治疗,保证充足的氧输送,避免机械通气造成的循环紊乱。下面简单总结刘大为教授提出的几点循环保护性通气策略要点:
1. 维持恰当的循环容量
这应该是最根本的。一个循环容量不足的患者,在机械通气甚至予镇静治疗后,可加剧低血压。提示我们要进行积极液体复苏。但过多的补液又会加重肺水肿。
刘大为教授指出:机械通气患者液体管理具有阶段性,疾病早期血管通透性升高,可导致容量不足,需要积极扩容,但后期病情控制后组织间隙水向血管内移动,则需要主动的进行液体负平衡,研究表明心功能不全和肺水肿是脱机失败的常见原因,但如果过多脱水又会导致组织灌注不足,导致病情反复。
动态把握液体管理十分重要。这也是我从事重症医学工作以来,上级医师时常对我提到的事情。
2. 确保充足的心输出量
某种程度上,机械通气对左心功能是有利的,因为机械通气减少静脉回流、降低前负荷等,因此,左心功能不全患者在撤离呼吸机时,需警惕脱机所致的心功能不全,在脱机前应根据血流动力学状态,给予相应的心功能保护措施:比如利尿、强心、控制心室率等。对右心而言,一般认为机械通气会加重右心功能不全。
刘大为教授建议:用重症超声技术早期发现机械通气时的肺高压和右心功能障碍,并强调连续右心功能评估指导ARDS机械通气治疗强度及策略。对于ARDS已合并急性肺心病患者,应尽可能避免导致气道平台压升高的通气措施(比如肺复张及高频通气),建议选择俯卧位通气等不增加气道平台压的方式进行右心保护,必要时ECMO治疗。
3. 避免血管张力的抑制
刘大为教授强调:在机械通气进行镇静镇痛治疗时,应注重其对血流动力学的影响,避免不恰当的药物治疗导致血流动力学不稳定。
但我们经常使用的咪达唑仑、丙泊酚、吗啡都可能导致低血压,尤其是在血容量不足、老年人更是如此。此外,在实施小潮气量肺保护通气策略时,可能导致严重的二氧化碳潴留及呼酸,进而外周血管扩张,血压下降等,但我们强调的是“允许性碳酸血症”,一旦“不允许”(如 pH 值低于 7.2),就要果断采取措施(增加通气量)。
4. 改善组织灌注
一般认为 CVP 是循环系统中的最低压力点,是器官保护的后向压力目标。高 CVP 会导致脑、肾、胃肠道等多器官水肿,严重影响器官的灌注。而 ARDS 患者有严重低氧血症时通常会采用较高的 PEEP,但后者会引起 CVP 升高。
刘大为教授建议:从保护组织灌注角度来讲,应避免高 PEEP 导致高 CVP。
综上所述,循环保护通气策略不仅仅是肺保护,更重要的是进行循环保护,实施循环保护性通气策略才能改善血流动力学及通气血流比例,提高氧输送,最终达到改善器官灌注和患者预后的目的。
通过以上我们发现,临床情况往往十分复杂,各系统、器官往往相互影响,我们要液体复苏,又要警惕肺水肿,我们要负平衡,但又不能危及组织灌注,我们要肺保护,但又不能过头导致严重酸中毒,我们要增加PEEP改善氧合,但又要避免低血压……我们就这样在夹缝中生存,在钢丝中欢舞。
中华内科杂志 2016年3月55卷3期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#小知识#
42
#环保#
42
讲的非常好
38
#重症患者#
25
讲的很全面
60
学习一下!
95
关注机械通气的同时,还要注意血液循环的有关问题。
59