Aging (Albany NY):糖尿病性视神经病变患者额中回高信号:低频波动的动态振幅研究
2022-02-21 从医路漫漫 MedSci原创
糖尿病(DM)是一种常见的慢性病,其患病率持续上升。
背景:糖尿病(DM)是一种常见的慢性病,其患病率持续上升。随着糖尿病的进展,神经病变已成为糖尿病患者最常见的并发症。糖尿病性视神经病变(DIN)是糖尿病的主要慢性并发症之一,包括糖尿病乳头病变、视盘新生血管、前部缺血性视神经病变和视神经萎缩。糖尿病视网膜病变(DR)患者中DON的患病率为38.4%。由于DON的形式多种多样,很难诊断,因此它会严重威胁糖尿病患者的视力,影响患者的生活质量,这突显了眼科医生评估的必要性。根据最近的报道,糖尿病患者的高血糖会减少局部组织血流量,这可能会影响视神经的新陈代谢。与DON相关的主要机制包括多元醇途径的激活、炎症反应和氧化应激。此外,随着疾病的发展,视神经会出现不可逆转的萎缩,最终导致失明。
目的:本研究的目的是利用低频波动的动态幅度(DALFF)探讨DON患者脑活动的动态变化。
总共有22名DON患者和22名健康对照者入选。在所有参与者中使用DALFF方法来研究两组之间动态内在脑活动的差异。
结果:与HCS组相比,DON组右侧额中回DALFF变异性显著增加(P<0.01)。相反,DON患者右侧楔前叶DALFF变异性明显降低(P<0.01)。DON患者右侧额中回HADS评分与DALF值呈显著负相关(焦虑r=0.6404,P<0.0 1;抑郁r=-0.6346,P<0.0 1;HADS、医院焦虑抑郁量表)。
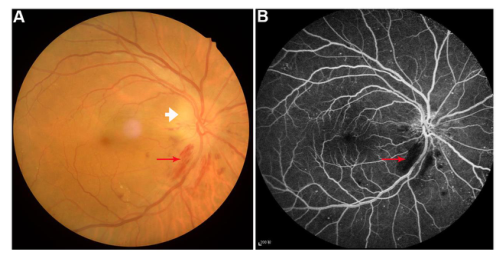
图1糖尿病视神经病变一例,行眼底照相(A)和荧光眼底血管造影(B)。观察视神经周围出血(红色箭头)和视盘水肿(白色箭头)。
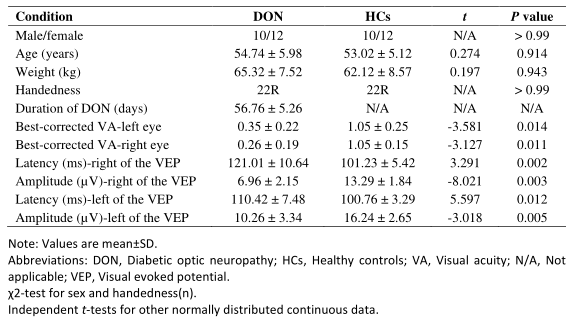
表1。本研究参与者的临床特征。
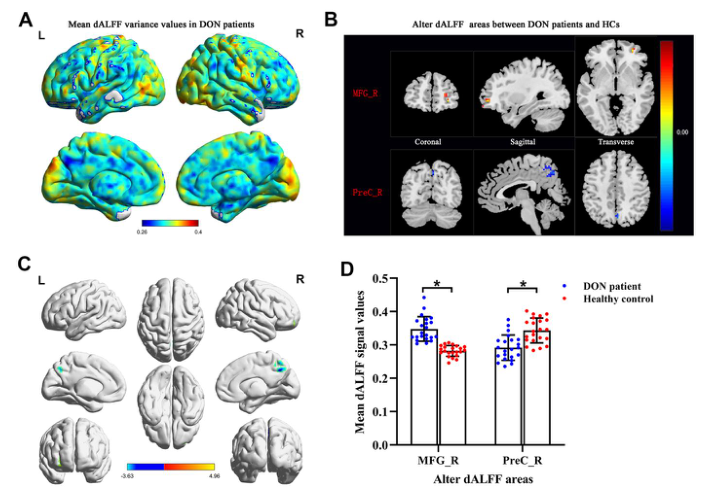
图2.DON患者和HCS患者之间不同dALF值的比较。观察了DON患者dALFF变异的空间分布模式。DON患者(A)的平均dALFF方差图。与HCS相比,DON患者MRG_R dALFF值增高,PREC_R dALFF值降低。它们在冠状位、矢状位和横位的代表性分布(B)和三维分布(C)。两组间的dALFF值比较采用双样本t检验。DON患者与HCS(D)患者之间改变的dALFF平均值。*代表P<0.01。暖色区域表示两组中较高的值,而冷色区域表示较低的值。缩写:dALFF,低频波动的动态幅度;DON,糖尿病视神经病变;HCS,健康对照;MFG,额中回;PREC,楔前;R,右;L,左。

表2.DON和HCS患者之间dALFF值显著不同的脑区
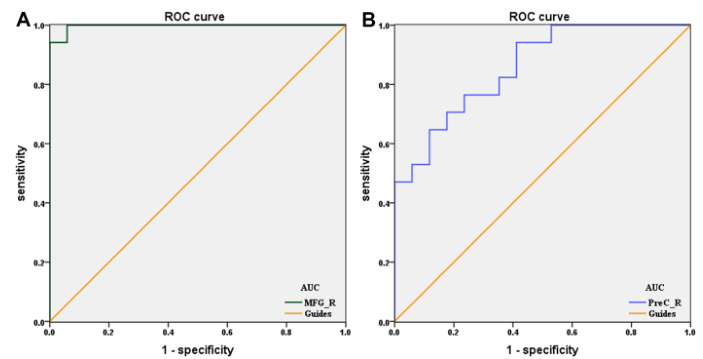
图3.改变的大脑区域的平均dALFF值的ROC曲线分析。(B)DON<HCS,PREC_R的ROC曲线下面积为0.858(P<0.0001;95%CI:0.737-0.979)。缩写:ROC,受试者工作特征;DALFF,低频波动的动态幅度;DON,糖尿病性视神经病变;HCS,健康对照;AUC,曲线下面积;R,右;
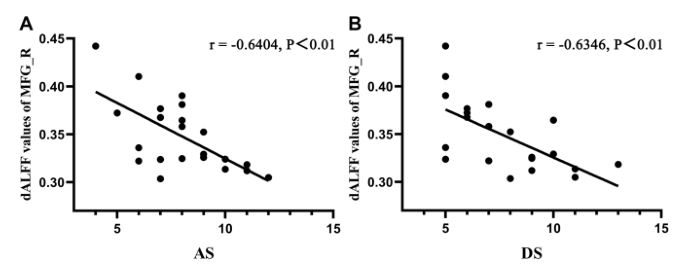
图4。MFG_R的dALFF值与临床行为的相关性。采用Pearson相关分析确定显著的dALF值与HDS评分之间的线性关系。焦虑评分与MFG_R的DALFF值呈负相关(r=−0.6406,P<0.0 1),抑郁评分与MFG_R的DALF值呈负相关(r=−0.6346,P<0.0 1)。缩写:dALFF,低频波动的动态幅度;MFG,额中回;R,右;AS,焦虑评分;DS,抑郁评分。
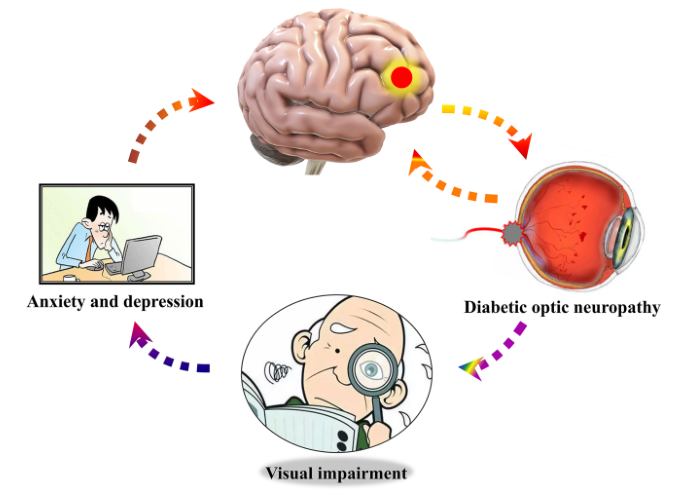
图5右侧额中回大脑dalff值与情绪状态的关系。与HCS相比,DON患者右侧额中回dALFF值降低,更易出现焦虑、抑郁情绪。缩写:dALFF,低频波动的动态幅度;HCS,健康对照组;DON,糖尿病视神经病变。
结论:在DON患者大脑特定区域观察到DALFF的异常变异,有助于鉴别DON和HCS,提高对DON的认识,右侧额叶中回高信号可能是诊断DON的潜在指标。
原文出处:Yang L, Xiao A, Li QY,et al.Hyperintensities of middle frontal gyrus in patients with diabetic optic neuropathy: a dynamic amplitude of low-frequency fluctuation study.Aging (Albany NY) 2022 Feb 04;14
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#视神经病变#
46
#视神经#
42
#高信号#
34
受益匪浅
61
学习
52
#神经病#
38
#神经病变#
61