Ann Thorac Surg:主动脉粥样硬化负担对主动脉瓣置换手术结果的影响
2020-08-18 MedSci原创 MedSci原创
主动脉外膜超声检测和定位升主动脉粥样硬化。在这项分析中,我们调查了手术主动脉瓣置换术(SAVR)期间基于主动脉超声的动脉粥样硬化等级与围手术期不良结局之间的关系。
主动脉外膜超声检测和定位升主动脉粥样硬化。在这项分析中,我们调查了手术主动脉瓣置换术(SAVR)期间基于主动脉超声的动脉粥样硬化等级与围手术期不良结局之间的关系。

在2种栓塞保护装置的随机试验中,SAVR患者在核心实验室进行了协议定义的5视点表皮超声检查。使用Katz动脉瘤等级量化主动脉粥样硬化,并将患者分为轻度(I-II级)或中度/重度(III-V级)。使用多变量logistic回归估计动脉瘤等级与不良结局之间的关联,包括7天和30天前的死亡、临床明显的卒中、弥散加权磁共振成像上的脑梗死、谵妄和急性肾损伤(AKI)。
结果显示,383例随机患者中的326例(85.1%)可获得插管前主动脉超声数据。其中106例(32.5%)在升主动脉的任何一段有中度/重度Katz动脉粥样硬化等级。尽管在7天的弥散加权磁共振成像上死亡、卒中或脑梗死的复合差异没有统计学意义,但中度/重度动脉瘤等级与7天前AKI的风险更大相关(校正后的OR,2.63;95%置信区间,1.24-5.58;P = .01)。30天时,中度/重度动脉瘤等级的患者有更大的死亡、卒中或AKI风险(校正后的OR,1.97;95%置信区间,1.04-3.71;P = .04)。
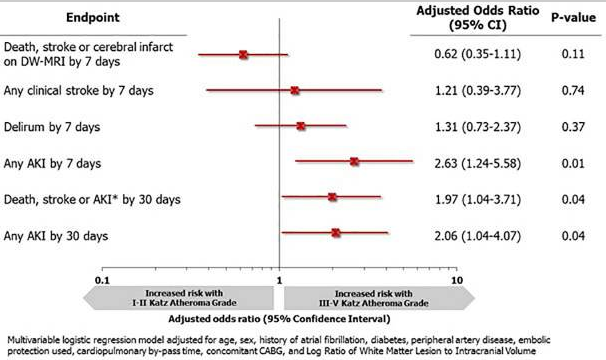
综上所述,该研究结果表明,中度/重度主动脉粥样硬化与SAVR后不良事件风险增加相关。主动脉外膜超声可作为一种有用的辅助手段,用于识别那些可能受益于SAVR期间减少动脉栓塞并发症的策略的患者。
原始出处:
Alexander Iribarne, Stephanie Pan, et al., Impact of Aortic Atherosclerosis Burden on Outcomes of Surgical Aortic Valve Replacement. Ann Thorac Surg. 2020 Feb;109(2):465-471. doi: 10.1016/j.athoracsur.2019.06.037.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#THORAC#
35
#粥样硬化#
0
#置换#
28
#主动脉瓣#
36
#主动脉#
30
赞
65