Cancer Discovery:细胞对CRISPR的应答不容忽视
2016-06-10 叶子 生物通
这两年几乎人人都在谈论CRISPR基因组编辑,那么细胞对这个系统的闯入作何感想呢?Cancer Discovery杂志最近发表的一项研究指出,细胞会对CRISPR-Cas9产生一种不容忽视的应答。 细菌一直在与病毒或入侵核酸进行斗争,为此它们演化出了多种防御机制,CRISPR-Cas适应性免疫系统就是其中之一。规律成簇的间隔短回文重复CRISPR与内切酶Cas9的组合,可以在引导RNA的指引
这两年几乎人人都在谈论CRISPR基因组编辑,那么细胞对这个系统的闯入作何感想呢?Cancer Discovery杂志最近发表的一项研究指出,细胞会对CRISPR-Cas9产生一种不容忽视的应答。
细菌一直在与病毒或入侵核酸进行斗争,为此它们演化出了多种防御机制,CRISPR-Cas适应性免疫系统就是其中之一。规律成簇的间隔短回文重复CRISPR与内切酶Cas9的组合,可以在引导RNA的指引下,靶标并切割入侵者的遗传物质。这种特性使CRISPR系统成为了基因组编辑和基因功能研究的实用工具。
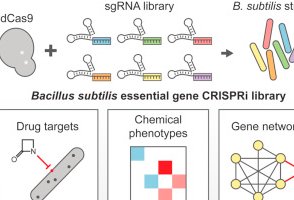
CRISPR-Cas9能够很方便的在哺乳动物细胞中进行体细胞遗传筛选。但哈佛大学Dana-Farber癌症研究所的科学家们在实践中发现,CRISPR-Cas9靶标会使细胞产生一种不依赖基因的应答。而这种应答会干扰人们对CRISPR筛选数据的解读。
为了鉴定增殖的必需基因,研究人员用CRISPR-Cas9在33个癌细胞系中进行了全基因组的功能缺失筛选。他们发现,基因组编辑之后的基因拷贝数增加和细胞活力下降有很强的关联。
在拷贝数增加的区域中,CRISPR-Cas9靶标会诱导G2细胞周期停滞,由此显著减少癌细胞的增殖。这项研究表明,被CRISPR-Cas9靶标的基因组引起了不依赖基因的抗增殖细胞应答。理解这种影响对于正确解读CRISPR-Cas9筛选数据非常重要。
基因筛选是经典的生物学研究方法,常用于鉴定在生物学过程中起作用的基因。十多年来RNAi一直是这一领域的王者,然而新兴技术的涌现(尤其是CRISPR技术)正在逐渐瓦解RNAi的统治地位。那么,在RNAi和CRISPR筛选之间我们究竟应该如何抉择呢?斯坦福大学的研究人员对这两种技术进行了全面比较,并将研究结果发表在Nature Biotechnology杂志上。
原始出处
Andrew J. Aguirre1, Robin M. Meyers2, Barbara A. Weir1, Francisca Vazquez1.et.al.Genomic copy number dictates a gene-independent cell response to CRISPR-Cas9 targeting.Cancer Discovery.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Dis#
36
#cover#
33
#CRISPR#
29
#ISC#
40
肿瘤免疫研究大有发展
112
值得研究
112
的确这样
93