Journal of Surgical Case Reports:18岁化生性乳腺癌一例
2015-01-21 hebe556 丁香园
近日,来自葡萄牙的Gomes教授等在Journal of Surgical Case Reports上报道了一例18岁少女罹患化生性乳腺癌">乳腺癌的病例。 案例 一名18岁的非洲女性患者因右乳直径34cm巨大肿瘤(图1)收住我院,既往无乳腺癌家族史。活检提示广泛坏死化生性乳腺癌,三阴性,Ki67>90%,胸腹部及骨盆CT提示腋窝淋巴结转移,其它未见明显转移。乳腺MRI提示肌肉浸润
近日,来自葡萄牙的Gomes教授等在Journal of Surgical Case Reports上报道了一例18岁少女罹患化生性乳腺癌">乳腺癌的病例。
案例
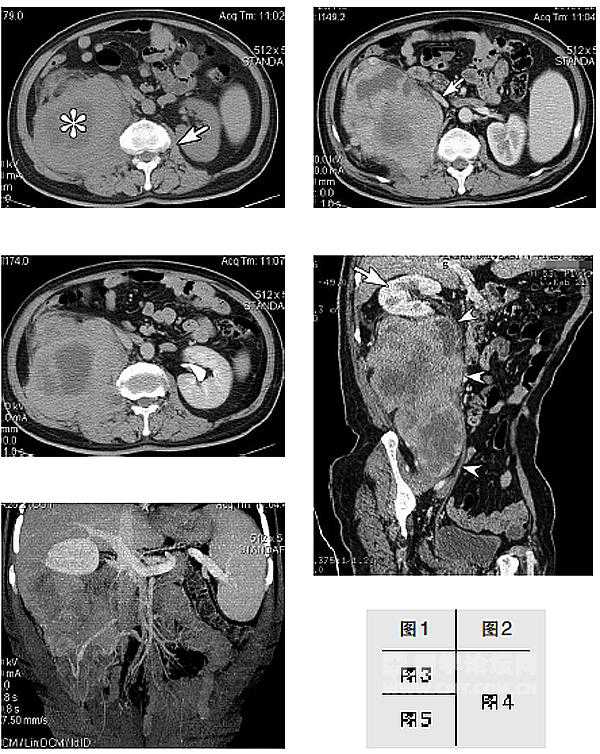
一名18岁的非洲女性患者因右乳直径34cm巨大肿瘤(图1)收住我院,既往无乳腺癌家族史。活检提示广泛坏死化生性乳腺癌,三阴性,Ki67>90%,胸腹部及骨盆CT提示腋窝淋巴结转移,其它未见明显转移。乳腺MRI提示肌肉浸润(图2)。多学科团队商讨后决定行右乳癌改良根治术(图3)。

图1 术前肿瘤外观

图2 MRI T1f显示巨大肿块占据整个右乳并呈中央区坏死

图3 手术标本
病理诊断化生梭形细胞癌(图4)。

图4 (A)4倍镜下可见血管外皮细胞瘤样所行增生(B)10倍镜下可见核多形性和大量的有丝分裂(C)10倍镜下可见集中表达CK903,提示上皮分化(D)10倍镜下可见波形蛋白高度及弥漫性表达
术后患者接受了4个疗程的阿霉素和环磷酰胺辅助治疗。术后6月,患者手术切口下出现了与胸壁黏连坚硬且伴疼痛的结节。B超提示9*7cm的异质性多囊性结节(图5)。胸部CT提示右侧胸腔积液,胸膜增厚和粘连。细胞学分析怀疑恶性细胞的存在。胸膜活检为阴性。

图5 超声显示乳房切除术床有一枚低回声实质性肿块并浸润胸大肌以下。
由于胸壁侵犯,无法进行再次切除,患者病情迅速恶化,很快出现多脏器功能衰竭。无进展生存率6个月,总生存率9个月。
关于化生性乳腺癌的思考
化生性乳腺癌是一种罕见、侵袭性强的乳腺恶性肿瘤,预后较差。MBC约占所有乳腺浸润癌的0.2%-5%,进展较快,多数发现时已是高级别的巨大肿瘤,较少淋巴结受累,三阴性、低分化或未分化,高Ki67。
化生性乳腺癌目前没有标准的治疗方案,我们遵循浸润性乳腺癌的临床实践指南行改良根治术联合化疗治疗。由于CT提示存在临床并发症、疾病复发及患者病情恶化等原因未行放疗。
由于患者入院太晚,以及低龄和种族原因,生存期低于均数。既往研究显示,不仅低龄女性容易罹患侵袭性高、分化低、ER阴性肿瘤,非洲女性更容易患低龄、高级别、ER阴性乳腺癌。
目前,化生癌仍缺乏有效的预后标志物。多学科参与下进行积极果断治疗为首要措施。虽然化生性乳腺癌较少见,但仍有相当一部分患者由于初级卫生保健欠缺,入院时已为晚期,因此,我们需要明确早期诊疗方案,以得到最佳治疗结果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








想知道是多久长成这么大的?
120
#case report#
35
#case#
32
太恐怖了,怎么会长这么大。
133
#Cas#
28