Cell:胰腺癌的潜在治疗靶标Lin28b被发现
2016-05-15 MedSci MedSci原创
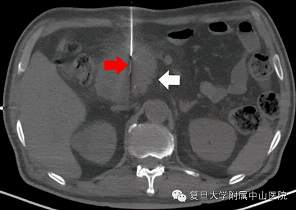
-在一项新的研究中,来自美国麻省总医院(MGH)等机构的研究人员鉴定出一种最为常见的被称作胰腺导管腺癌(pancreatic ductal adenocarcinoma, PDAC)的胰腺癌类型的首个潜在的分子治疗靶标。除了发现在大约30%的PDAC病例中肿瘤抑制蛋白SIRT6失活之外,研究人员还鉴定出SIRT6抑制PDAC发展的精确分子机制,这一机制不同于它抑制结直肠癌的方式。相关研究结果于

-在一项新的研究中,来自美国麻省总医院(MGH)等机构的研究人员鉴定出一种最为常见的被称作胰腺导管腺癌(pancreatic ductal adenocarcinoma, PDAC)的胰腺癌类型的首个潜在的分子治疗靶标。除了发现在大约30%的PDAC病例中肿瘤抑制蛋白SIRT6失活之外,研究人员还鉴定出SIRT6抑制PDAC发展的精确分子机制,这一机制不同于它抑制结直肠癌的方式。相关研究结果于2016年5月12日在线发表在Cell期刊上,论文标题为“SIRT6 Suppresses Pancreatic Cancer through Control of Lin28b”。
论文通信作者、MGH癌症中心科学家Raul Mostoslavsky博士说,“随着癌症基因组学取得的进展,表观遗传因子---控制其他基因是否和何时表达的那些基因-发生的变化很明显代表着癌症内最为频繁发生的变化中的一些。然而,在此之前,人们很少描述过这些因子,而且已被鉴定出的那些因子也未与特异性的下游靶标相关联。在分析的PDAC病人样品中,30%以上的样品表现出我们鉴定出的分子特征,而且这些病人也经证实具有很差的预后。”
已知SIRT6控制细胞加工葡萄糖的方式,而且Mostoslavsky团队在2012年的一项研究中已发现它抑制结直肠癌的能力涉及控制一种被称作醣酵解的过程。尽管那项研究也发现SIRT6在PDAC肿瘤细胞中下降表达,但是当前的这项新研究表明SIRT6缺乏通过一种不同的机制促进PDAC发展。针对细胞系和模式动物的实验揭示出PDAC中的低水平SIRT6与Lin28b增加表达相关联,其中Lin28b是一种在胎儿发育期间正常表达的癌蛋白。
Lin28b表达经证实是SIRT6缺乏的PDAC肿瘤细胞生长和存活所必不可少的,而且它的作用机制阻止被称作let-7的肿瘤抑制mRNA家族阻断三种基因HMGA2、IGF2BP1和IGF2BP3的表达,其中之前已知这三种基因与胰腺癌增加的侵袭性和转移相关联。所有的这些特征---下降表达的SIRT6、增加表达的Lin28b和下降表达的let-7---在更早死亡的病人PDAC肿瘤样品中发现到。
在未来,研究人员希望开发Lin28b抑制剂可能让这一部分PDAC病人受益,因为当前这些病人只有非常少的治疗选择。
原始出处:
Sita Kugel, Carlos Sebastián, Julien Fitamant, Kenneth N. Ross, Supriya K. Saha, Esha Jain, Adrianne Gladden, Kshitij S. Arora, Yasutaka Kato, Miguel N. Rivera, Sridhar Ramaswamy, Ruslan I. Sadreyev, Alon Goren, Vikram Deshpande, Nabeel Bardeesy, Raul Mostoslavsky. SIRT6 Suppresses Pancreatic Cancer through Control of Lin28b. doi:10.1016/j.cell.2016.04.033
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#LIN28#
37
#Cell#
31
#CEL#
25
拜读,好文
61
#治疗靶标#
35
#靶标#
26
很前沿的进展
113
发现不断
74