Chest:支气管超声引导下针吸穿刺(EBUS-TBNA)获得的标本检测PD-L1表达同样可指导PD1抑制剂在晚期NSCLC患者中的应用
2021-12-24 yd2015 MedSci原创
研究表明,EBUS获得标本以及传统获取组织标本检测PD-L1表达对于指导PD-1抑制剂治疗晚期NSCLC患者的疗效无明显差异。
晚期肺癌有研究表明PD-L1的检测在支气管超声引导下针吸穿刺(EBUS-TBNA)获得的标本中是可行的。但是EBUS获得标本以及传统获取组织标本检测PD-L1表达对于指导PD-1抑制剂治疗的疗效有无差异,目前仍不明确。因此,有来自加拿大的团队开展了相关研究,评估EBUS获得标本以及传统获取组织标本检测PD-L1表达对于指导PD-1抑制剂治疗晚期NSCLC患者的疗效有无差异。相关研究成果发表在Chest杂志上。
2016年6月至2019年6月期间接受pembrolizumab或nivolumab治疗的患者被纳入研究。收集患者特征、PD-L1表达、治疗线数、疗效。评估无进展生存期(PFS)和总生存期(OS)。
共纳入145例患者,其中EBUS-TBNA 46例(31.7%)和组织学标本组99例(68.3%)。患者平均年龄为66.8 ?9.1岁,女性71例(49.0%)。大多数在ICI开始时有转移性疾病以及ECOG为0 ~ 1。EBUS-TBNA组非鳞状组织的患者比例较高,89.1% vs 65.7% (P=0.003)。两组的PD-L1TPS水平类似,总体62.8%患者PD-L1 TPS ≥50%。一线pembrolizumab用于61名PD-L1 TPS≥50%患者,其中EBUS-TBNA组16例,或组织学样本组45例。
中位随访11个月,90例患者死亡,其中EBUS-TBNA 29例(63%),组织学标本组61例(61.6%)。不管免疫治疗的线数,总体人群的中位PFS和OS分别为6.6个月(95% CI, 4.1-8.8)和12.5个月(95% CI 9.1-17.8)。61例一线pembrolizumab治疗患者中,两组的中位OS分别为25.8个月(95% CI 6.5 to not reached)和未达到(95% CI, 9.14 to not reached),没有统计学差异(HR, 0.82[95% CI, 0.34-1.95], P=0.651)。两组的中位PFS分别为15.2个月(95% CI, 3.3 to not reached)和11.9个月(95% CI, 4.01 to not reached),同样没有统计学差异(HR, 0.78 [95% CI, 0.35-1.73], P =0.538)。
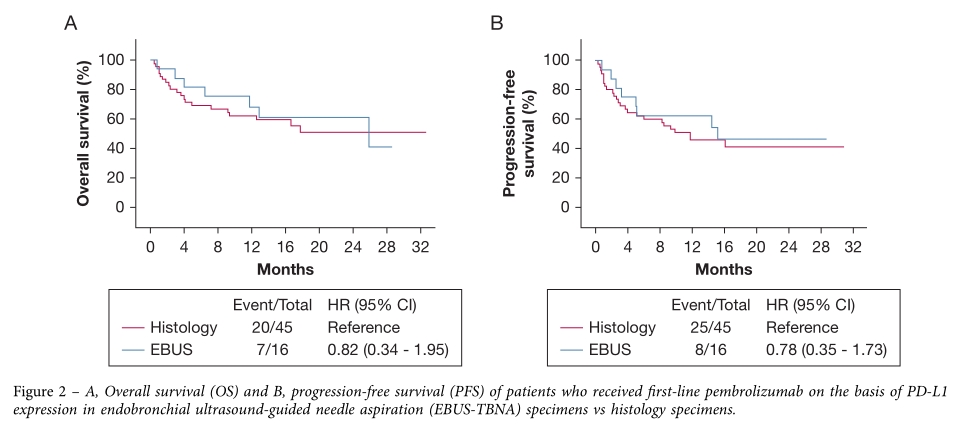
一线pembrolizumab治疗两组的预后差异
后线接受pembrolizumab或nivolumab治疗患者中,两组的中位PFS(HR= 0.89,95%CI,0.54 - 1.46)和OS(HR=0.98,95%CI, 0.58 - 1.64)均没有统计学差异。
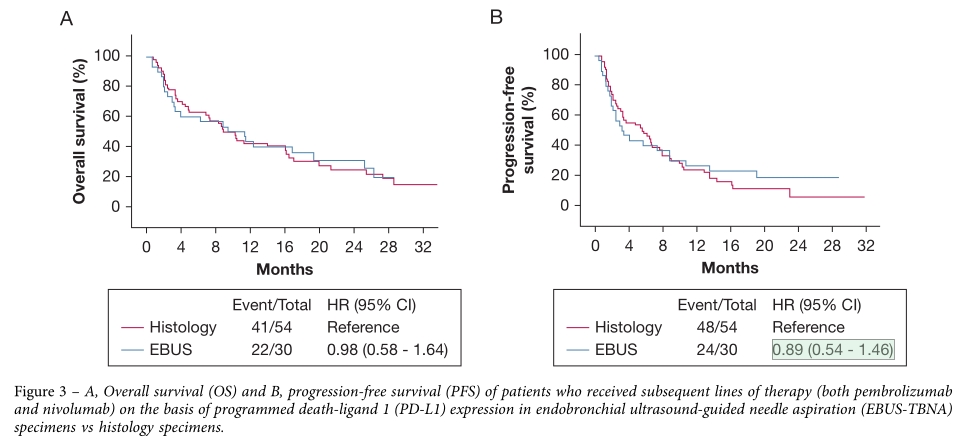
后 线ICI治疗两组的预后差异
对年龄、性别、分期、PD-L1表达水平、病理组织类型(鳞癌 vs 非鳞癌)、CNS转移状态或吸烟状态等进行亚组分析发现,两组的PFS和OS同样没有统计学差异。

亚组分析预后差异
综上,研究表明,EBUS获得标本以及传统获取组织标本检测PD-L1表达对于指导PD-1抑制剂治疗晚期NSCLC患者的疗效无明显差异。
原始出处:
Tajarernmuang P, Ofiara L, Beaudoin S, Wang H, Benedetti A, Gonzalez AV. Real-World Outcomes of Patients With Advanced Non-small Cell Lung Cancer Treated With Anti-PD1 Therapy on the Basis of PD-L1 Results in EBUS-TBNA vs Histological Specimens. Chest. 2021 Aug;160(2):743-753. doi: 10.1016/j.chest.2021.02.053. Epub 2021 Mar 3. PMID: 33675792.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EBUS-TBNA#
45
#标本#
46
#超声引导#
35
#PD1抑制剂#
49
#抑制剂#
47
#超声引#
34
#Chest#
39
#SCLC患者#
26
#支气管#
41
#PD-L1表达#
27