肺动脉段明显突出 就是肺动脉高压吗?
2017-11-23 佚名 环球医学
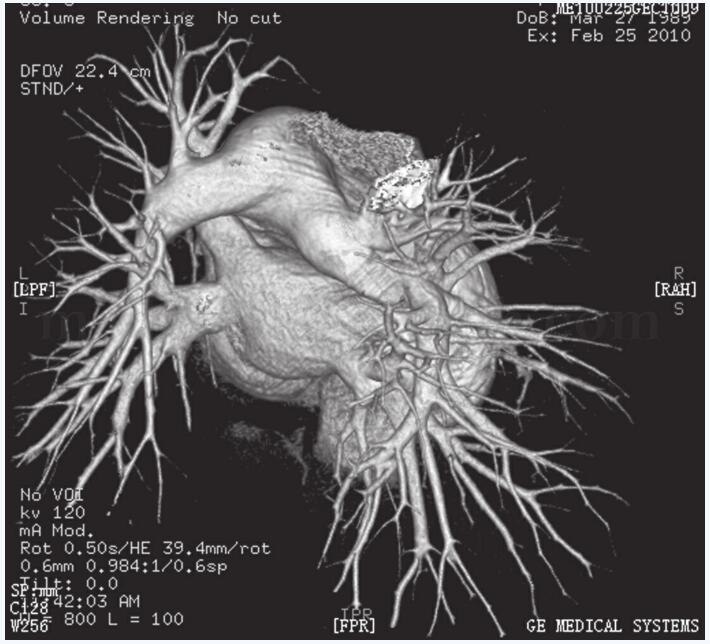
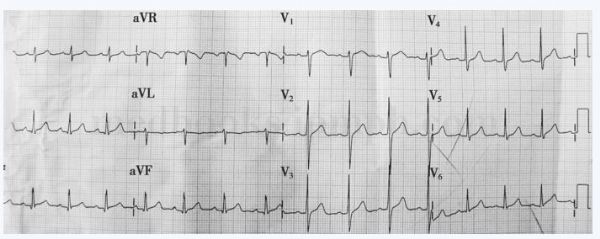
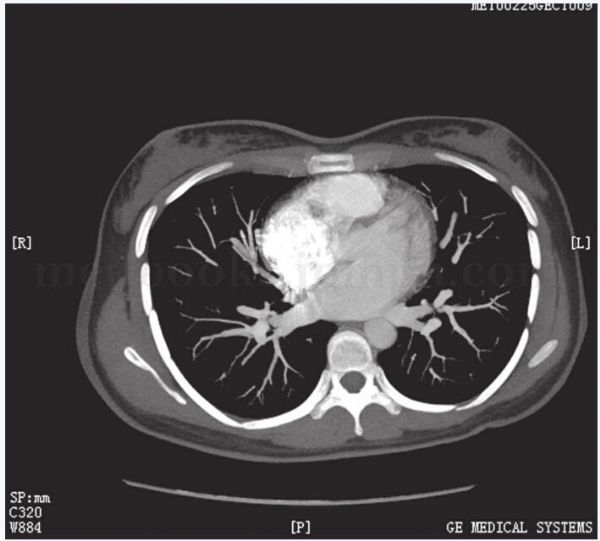
特发性肺动脉扩张(IDPA)是一种比较少见的疾病,一般不需要治疗,预后良好。由于许多先天性和获得性心血管疾病均可引起肺动脉扩张,容易误诊,因此,正确鉴别IDPA和继发性肺动脉扩张有重要的临床意义。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
37
学习一下
71
学习了谢谢分享!!
69
学习
58
学习了.涨知识
71
好病例.学习了.
61
学习了.谢谢分享
25