Brain Behav Immun:振奋人心!老药新用,抗炎药可有效对抗脑卒中,促进脑细胞再生
2016-11-29 MedSci MedSci原创
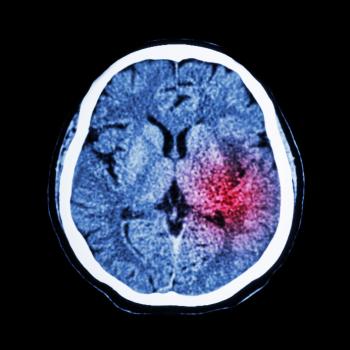
全球内脑卒中是导致死亡和残疾的第二大原因,卒中后会阻断大脑中的血液流动破坏脑细胞。现在,来自英国曼彻斯特大学的一项新的研究表明,一种已经批准用于治疗其他疾病的药物不仅可限制卒中的危害还可促进脑细胞的修复。在大鼠中,研究人员已证实该药物可减少脑细胞的死亡数量,并刺激新的脑细胞的产生,该研究结果已发表于Brain, Behavior, and Immunity。该研究探究了缺血性脑卒中,当机体发生缺血
脑卒中是世界上导致死亡和残疾的第二大原因,卒中后会阻断大脑中的血液流动破坏脑细胞。现在,来自英国曼彻斯特大学的一项新的研究表明,一种已经批准用于治疗其他疾病的药物不仅可限制卒中的危害还可促进脑细胞的修复。
在大鼠中,研究人员已证实该药物可减少脑细胞的死亡数量,并刺激新的脑细胞的产生,该研究结果已发表于Brain Behavior and Immunity。
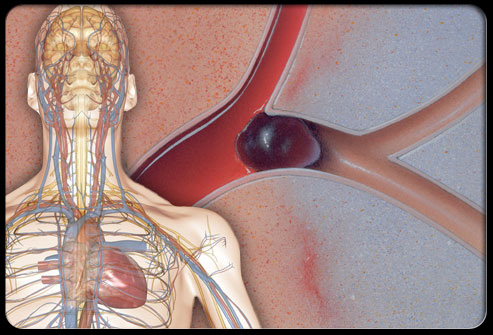
该研究探究了缺血性脑卒中,当机体发生缺血性脑卒中时,可阻断给大脑供应氧气的动脉血。
研究人员在脑卒中小鼠中使用了一种抗炎药——IL-1受体拮抗剂(IL-1Ra)。结果发现,IL-1Ra不仅可在卒中早期阶段减少脑损伤,还可在大鼠卒中后几天内促进新的脑细胞(神经元)数量的增加。而且这一效果与小鼠的年龄及胖瘦无关。
研究人员指出,虽然卒中本身也可以引发机体损伤后的一个强大的修复反应,但是许多新产生的细胞并不能整合至原有的脑神经系统中。
当研究人员分析IL-1Ra对大鼠大脑神经元再生的影响时,他们发现,该药不仅可促进干细胞的增殖,还能显著提高脑缺血后神经细胞的迁移,并显著增加新生神经元的数目。
既往研究因无法处理脑卒中中所发生的炎症反应,因此无法将其实验室发发现的药物成功应用与临床,现在这个实验结果为IL-1Ra的使用提供了强有力的支撑,不过未来仍需进一步的大规模临床试验研究以探究该药在人体内的效果。
原始出处:
[1] Catharine Paddock PhD.Stroke: New drug limits brain damage and promotes repair. MNT.28 November 2016.
[2] Jesus M. Pradillo et al., Reparative effects of interleukin-1 receptor antagonist in young and aged/co-morbid rodents after cerebral ischemia. Brain Behav Immun. 2016 Nov 14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#HAV#
48
好资料,值得学习
77
了解一下
100
#抗炎药#
47
#脑细胞#
38
#EHA#
0
看到了希望,棒棒的
84
可以更加适合运用到临床
73