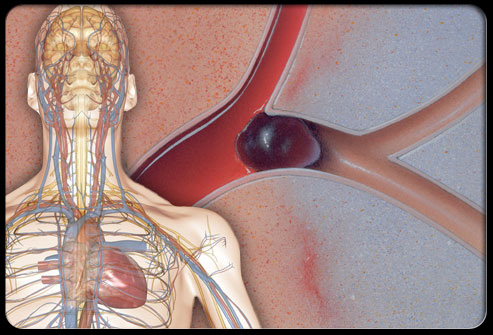
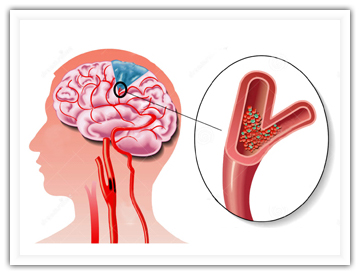
Neurology:急性脑卒中患者鼻饲管与肺炎、临床结局的关系
2016-10-01 xing.T MedSci原创
由此可见,早期插入鼻饲管不会增加卒中后肺炎发病率、死亡率和较差功能预后,它可安全用于急性卒中患者。
近日,神经病学领域权威杂志《neurology》上发表来自英国伦敦国王学院附属医院临床和基础神经科学系Lalit Kalra博士及其团队的文章,旨在明确急性脑卒中患者鼻饲管、肺炎及其临床结局的关系。
该研究是一项多中心的随机对照试验,纳入了从2008年4月21日至2014年5月17日期间住院1217例在症状发作48小时内预防性运用抗生素并且限制进食的卒中患者,在第14天,研究者分析了卒中后肺炎的发生情况,以及在第90天评估患者死亡率和采用改进的Rankin量表评分系统来衡量功能。采用广义混合模型对年龄、合并症、卒中类型、严重程度以及护理质量进行调整。在后续的14天所有患者都有随访,而在90天有36(3%)例未进行随访。
研究者发现插有鼻饲管的患者(298/1217[24.4%])有更严重的卒中(中位NIH卒中量表评分17 vs 14,P=0.0001)、意识障碍(39% vs 28%,P=0.001)。
由此可见,早期插入鼻饲管不会增加卒中后肺炎发病率、死亡率和较差功能预后,它可安全用于急性卒中患者。
原始出处:
Lalit Kalra,et al. Association between nasogastric tubes, pneumonia, and clinical outcomes in acute stroke patients. Neurology. 2016.Sep 27;87(13):1352-9.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Neurol#
54
#临床结局#
46
#卒中患者#
43
#脑卒中患者#
50
#急性脑卒中#
48
继续关注
86
继续学习
77
证据出来了
71