主动脉夹层,这一危急重症,是从无到有瞬间发生,还是像癌症那样有个进展过程的呢?
我以前一直以为,主动脉夹层是瞬间发生的。大部分关于主动脉夹层的描述,都会说,该病,是血流冲破内膜,导致内膜分层形成,感觉血流冲破内膜,那肯定是瞬间发生的。
或者有些文献会介绍主动脉夹层可能的另有机制是,中膜形成血肿,然后向内膜破溃,致血流由内膜破口进入中膜导致中膜分离并扩展。不管是以上哪个机制,最后结果是,主动脉壁形成真假两腔。
2011年,我逐字逐句翻译了美国2010版的胸主动脉疾病诊治指南(ACCF/AHA/AATS /ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic diseas)的大部分,当读到其中论述主动脉夹层的定义时,讲述了Svensson分型。
该分型由美国克利夫兰诊所的Lars Svensson医生提出,其主要依据是他做以千计的主动脉手术后关于主动脉夹层的理解。

图1:Svensson分型
I型:典型夹层的内膜撕裂伴真假腔形成,真假腔形成间隔,但两腔之间可见交通,最常见于降主动脉肋间动脉分出部位。
II型:壁内血肿,影像学上未见内膜撕裂及间隔,但可通过手术和尸检发现。
III型:内膜撕裂而无中膜血肿形成,即局限性夹层,为主动脉壁的反常膨出,较罕见,难以通过CT或经食管超声心动图发现,较多见马方综合征,可致主动脉破裂出血。
IV型:穿透性主动脉溃疡,多穿透至外膜并形成囊状动脉瘤,发生于升主动脉和主动脉弓的穿透性溃疡多进展成I型主动脉夹层。
V型:医源性或创伤性主动脉夹层,前者多为行导管血管造影操作的并发症,后者多发生于急剧减速时。
其他4型,我都能理解,因为我既看到过术中所见,也收集了一些影像学资料,但我很难理解III型。如果血流可以造成内膜破裂,怎么还能对中膜手下留情?
去查文献,即使是今天我用“(Svensson)AND (主动脉)”这一检索式在万方上检索,切题的中文文献基本为零。当然英文文献也不太多,也许真的比较罕见吧。当然这个问题一直困扰着我,慢慢的碰到了一些病例,有了一些体会。Svensson大师诚不欺我,分享一例。
病例分享
患者,男,63例。因胸闷3月入院,术前评估后,因巨大升主动脉瘤累及根部、二叶式主动脉中重度关闭不全并轻度狭窄行BENTALL术。
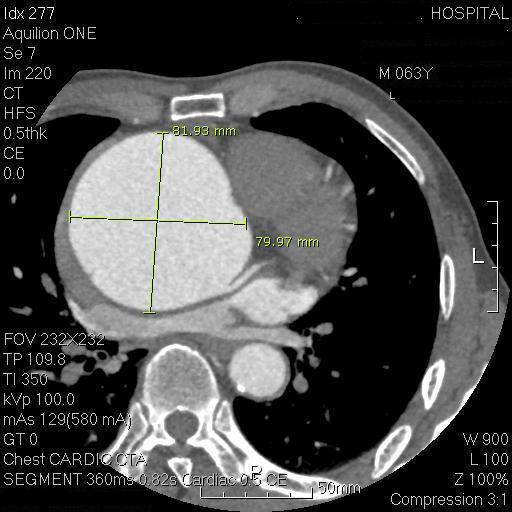
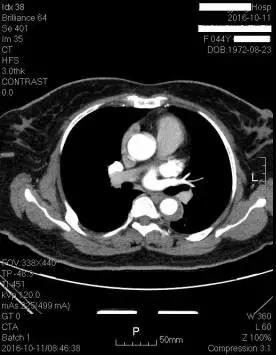
图2:主动脉根部最大直径8厘米
开胸后,巨大主动脉瘤不意外(图3),但蓝色方框中的那一抹蓝,有点奇怪。(抱歉,手机拍摄,对焦不够准确,且主动脉表面有反光,这抹蓝不够显着,术中肉眼是看得很显着的。)
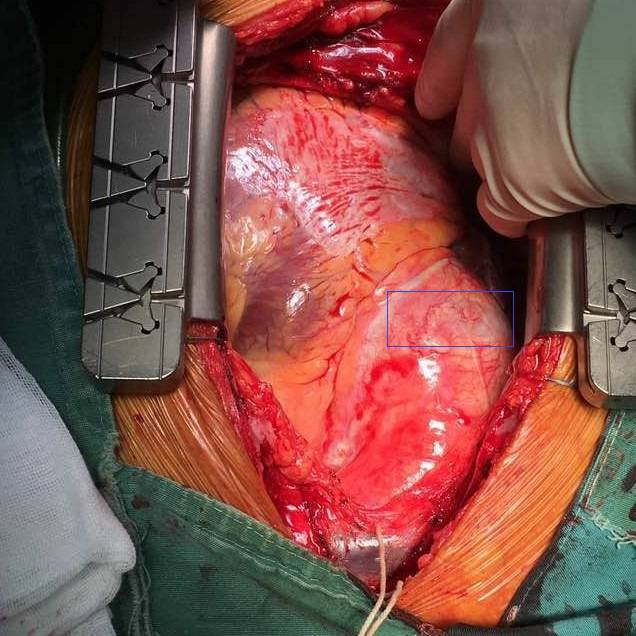
图3
切开主动脉壁,竟然发现这抹蓝是因为内膜破裂造成!(再次抱歉,手机拍摄,且本频道有不少大众读者,故不展示。)
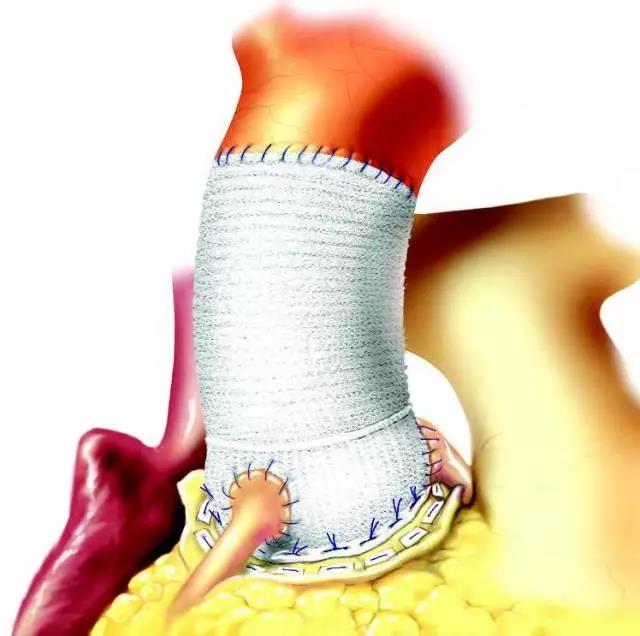
术中切下一片主动脉壁,清洗干净,很明显(图4),可以看到上图中部局部主动脉壁内膜破裂显出的那摸蓝是因为此处主动脉壁较周围薄弱所致。这就是一例Svensson III型主动脉病变。
图4
这种征象,我在多例马凡综合征患者巨大根部瘤的病例中见过,这例临床评估,无马凡综合征表现,但具有二叶式主动脉瓣,目前也有不少资料显示二叶式主动脉瓣者,也如马凡综合征其主动脉壁是薄弱的。
可以合理推断,该例如继续进展,将很快转变为典型的主动脉夹层。所幸,BENTALL术及时终止了这一过程。
术后CT重建,手术治疗效果良好
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了谢谢分享
77
学习并分享!!
71
#主动脉#
42
#动脉夹层#
45
学习了很多先进的医疗技术
69
学习学习.了解了解
74
学习了很有用
68