《急性心衰院前和院内早期管理指南》发布及要点
2015-05-29 大鹏 译 医学论坛网
5月21日,《欧洲心脏杂志》(European Heart Journal)刊发了由欧洲心脏学会(ESC)心力衰竭委员会、欧洲急诊治疗学会和流行病学急诊治疗学会联合制定的《急性心力衰竭院前和院内早期的管理指南》(简短版本). 一、急性心衰早期诊疗指南之病房治疗要点 病房治疗及ICU/CCU治疗要点 1.若患者存在显著呼吸困难或血流动力学不稳定状态,应将患者安置于可立即开展心肺复
5月21日,《欧洲心脏杂志》(European Heart Journal)刊发了由欧洲心脏学会(ESC)心力衰竭委员会、欧洲急诊治疗学会和流行病学急诊治疗学会联合制定的《急性心力衰竭院前和院内早期的管理指南》(简短版本).
一、急性心衰早期诊疗指南之病房治疗要点
病房治疗及ICU/CCU治疗要点
1.若患者存在显著呼吸困难或血流动力学不稳定状态,应将患者安置于可立即开展心肺复苏的场所。
2.急性心衰患者需针对性专科护理及诊疗。
3.推荐高危患者入CCU专科治疗,另外急性心衰伴急性冠脉综合征患者亦需转诊入CCU治疗,具体内容如下:
临床风险评估可辅助确定患者急诊之后是否需最高水平入院诊疗;
急诊特定评估法可进一步确定患者是否需要入ICU/CCU;
入ICU标准包括呼吸频率>25、SaO2<90%、存在辅助肌呼吸现象、收缩压<90mmHg;
需转诊ICU标准包括需气管插管(或已插管)或低灌注征象,后者包括少尿、四肢厥冷、精神状态异常、乳酸>2mmol/L、代谢性酸中毒及SvO2<65%。
4.若患者进入ICU/CCU治疗,其后续治疗(ICU/CCU之外的治疗)尽可能在心内科病房完成。
5.应设置急性心衰患者绿色通道。
院内监测注意事项
1.患者需每天称重,并有准确的体液平衡记录表。
2.给予标准无创监测,指标包括脉搏、呼吸频率和血压。
3.每天检测肾功能及电解质情况;
4.出院前检测钠尿肽有助于制定出院后治疗方案。
出院标准及高危患者随访
1.下列急性心衰患者符合出院标准:
出院前24小时血流动力稳定、容量正常、有循证医学口服治疗且肾功能正常;
已被告知自我护理相关内容。
2.对于出院的急性心衰患者,应做到以下几点:
入组疾病管理系统;
出院一周内主治医生随访;
如有条件,出院两周内心脏病学的团队随访。
3.慢性心衰患者应给与多专科心衰随访。
心源性休克诊疗要点
1.心源性休克定义为尽管积极补液,但仍存在低血压(SBP<90 mmHg)及低灌注的疾病表现。
2.对于疑似心源性休克的患者,应立即进行心电图及心脏超声检查。
3.需动脉导管有创监测。
4.监测心源性休克患者血流动力学状态的最佳方式尚无定论。
5.如果患者无容量负荷,推荐溶液冲击作为一线疗法。
6.可使用多巴酚丁胺增加心输出量,可考虑左西孟坦,尤适用于口服β受体阻滞剂的慢性心衰患者。
7.无特殊情况,可使用血管加压药,去甲肾上腺素优于多巴胺。
8.及时转诊至专科机构。
9.不推荐给予主动脉球囊扩张。
10.难治性心源性休克可考虑短期机械循环治疗,且暂不确定何种机械循环更优。
二、急性心衰院前及院内早期管理指南之药物和机械治疗要点篇
病房治疗及ICU/CCU治疗要点
1.若患者存在显著呼吸困难或血流动力学不稳定状态,应将患者安置于可立即开展心肺复苏的场所。
2.急性心衰患者需针对性专科护理及诊疗。
3.推荐高危患者入CCU专科治疗,另外急性心衰伴急性冠脉综合征患者亦需转诊入CCU治疗,具体内容如下:
临床风险评估可辅助确定患者急诊之后是否需最高水平入院诊疗;
急诊特定评估法可进一步确定患者是否需要入ICU/CCU;
入ICU标准包括呼吸频率>25、SaO2<90%、存在辅助肌呼吸现象、收缩压<90mmHg;
需转诊ICU标准包括需气管插管(或已插管)或低灌注征象,后者包括少尿、四肢厥冷、精神状态异常、乳酸>2mmol/L、代谢性酸中毒及SvO2<65%。
4.若患者进入ICU/CCU治疗,其后续治疗(ICU/CCU之外的治疗)尽可能在心内科病房完成。
5.应设置急性心衰患者绿色通道。
院内监测注意事项
1.患者需每天称重,并有准确的体液平衡记录表。
2.给予标准无创监测,指标包括脉搏、呼吸频率和血压。
3.每天检测肾功能及电解质情况;
4.出院前检测钠尿肽有助于制定出院后治疗方案。
出院标准及高危患者随访
1.下列急性心衰患者符合出院标准:
出院前24小时血流动力稳定、容量正常、有循证医学口服治疗且肾功能正常;
已被告知自我护理相关内容。
2.对于出院的急性心衰患者,应做到以下几点:
入组疾病管理系统;
出院一周内主治医生随访;
如有条件,出院两周内心脏病学的团队随访。
3.慢性心衰患者应给与多专科心衰随访。
心源性休克诊疗要点
1.心源性休克定义为尽管积极补液,但仍存在低血压(SBP<90 mmHg)及低灌注的疾病表现。
2.对于疑似心源性休克的患者,应立即进行心电图及心脏超声检查。
3.需动脉导管有创监测。
4.监测心源性休克患者血流动力学状态的最佳方式尚无定论。
5.如果患者无容量负荷,推荐溶液冲击作为一线疗法。
6.可使用多巴酚丁胺增加心输出量,可考虑左西孟坦,尤适用于口服β受体阻滞剂的慢性心衰患者。
7.无特殊情况,可使用血管加压药,去甲肾上腺素优于多巴胺。
8.及时转诊至专科机构。
9.不推荐给予主动脉球囊扩张。
10.难治性心源性休克可考虑短期机械循环治疗,且暂不确定何种机械循环更优。
三、急性心衰院前及院内早期管理指南之入院诊断篇
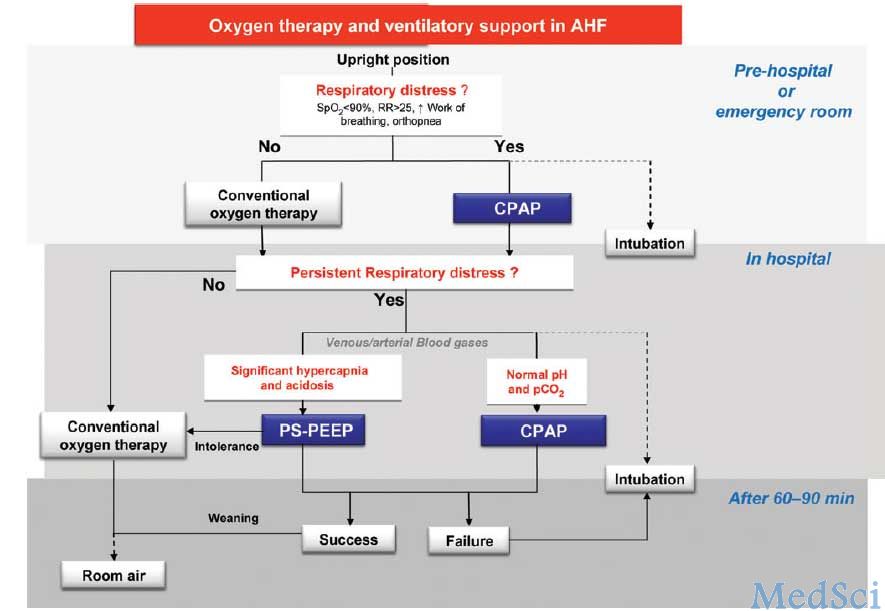
急性心衰院前及早期治疗策略
1.若急性心衰患者出现急性冠脉综合征,应秉承“及时治疗”理念治疗。所有急性心衰患者均应尽早接受适宜的治疗
2.对于处于院前阶段的急性心衰患者,下列措施能带来治疗收益:
尽早开展无创监测(如急救车内),包括脉搏血氧饱和度、血压、呼吸频率及连续心电监测等;
若患者氧饱和度<90%,氧疗法应纳入常规治疗,除此之外的情况均需根据临床诊断决定是否氧疗;
给予呼吸窘迫患者无创通气;
根据患者血压情况和/或充血程度决定是否给予药物治疗,一般考虑血管扩张剂、利尿剂;
尽快转诊至附近有完备心内科和/或CCU/ICU的大中型医院。
3.一旦患者进入急诊/CCU/ICU,需立即同时开展体检、调查及治疗工作。
如何完善入院临床评估及临床调查
1.对于疑似急性心衰患者,首先根据患者呼吸困难程度、血流动力学状态及心律判断患者心肺功能不稳定严重度,需记录以下检测结果:
呼吸困难严重度,包括呼吸频率、是否能仰卧、呼吸力度及缺氧程度;
血压(舒张期及收缩期);
心律及心率;
体温情况,是否存在低灌注征象(如四肢阙冷、脉压变窄或精神淡漠)。
2.继续评估患者是否存在充血,包括外周水肿情况、是否有啰音、静脉压是否升高等。
3.可能用到的额外检测:
心电图,虽然急性心衰患者很少有正常表现,但可以鉴别诊断ST段抬高型心电图;
实验室检查(见下);
床旁胸部超声,诊断是否有间质水肿,腹部超声检查下腔静脉直径及水肿情况;
胸片,鉴别诊断。
4.除非患者出现血流动力学不稳定状态,否则多数不需要起始超声心动检查,但需在后续检测中开展。
5.尽量避免导尿术。
急性心衰实验室检查
1.所有患者均需检查血浆钠尿肽水平(BNP、 NT-proBNP或 MR-proANP)以鉴别非心因性呼吸困难。
2.入院患者取血后应立即完成下列检测:肌钙蛋白、BUN(或尿素)、肌酐、电解质、血糖和全血细胞计数。
3.疑似急性肺栓塞需D-二聚体检测;
4.除非有特殊需要,否则不需常规动脉血气检查。
心衰诊治评估流程图
下载原文PDF:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














原则性的概述,个体化的治疗,纠正病因、去除诱因是关键,急则治其标,缓则治其本。
116
#管理指南#
24
#院前#
39
看看
96
#急性心衰#
45
#早期管理#
33
很有用
108