JAMA Netw Open:试管婴儿患癌风险比自然生产增加200%!出生缺陷比例也更高
2020-11-05 Bio生物世界 Bio生物世界
“试管婴儿”对于很多人来说虽然操作上很陌生,但是我们还是或多或少听过这一辅助生殖技术。对于想生育孩子的父母来说,“试管婴儿”圆了很多人当父母的梦想。
“试管婴儿”对于很多人来说虽然操作上很陌生,但是我们还是或多或少听过这一辅助生殖技术。对于想生育孩子的父母来说,“试管婴儿”圆了很多人当父母的梦想。从1978年第一个试管婴儿在英国诞生以来,这一技术发展至今已经相当完善。根据美国2017年的数据显示,当年出生的胎儿中,大概有2%的胎儿是通过试管婴儿孕育而来。
但是伴随着新技术而来的,还有一些隐藏的风险,而随着试管婴儿越来越多,这些潜在的风险或许会不断地暴露出来。
2020年10月29日,JAMA 子刊 JAMA Network Open 杂志发表了一项题为:Assessment of Birth Defects and Cancer Risk in Children Conceived via In Vitro Fertilization in the US 的研究论文。
这项大型研究发现,试管婴儿出生缺陷和患癌风险都要比自然分娩的胎儿更高,这个数据可以相差达200%。
根据研究团队的数据,他们一共选取了美国四个州的儿童数据,包括:马萨诸塞州、纽约、北卡罗来纳州和得克萨斯州,对自然生产的儿童和试管婴儿就出生缺陷和癌症进行了队列研究,其中包括1000639名孕妇自然生产的儿童和52776名通过试管婴儿技术生产的儿童。
这项研究的时间跨度也是相当之久,在4个州的跟踪时间均从2004年开始,最晚到2016年结束,对于儿童的随访时间平均可达5.7年,对于这些儿童的数据分析就长达5个月。
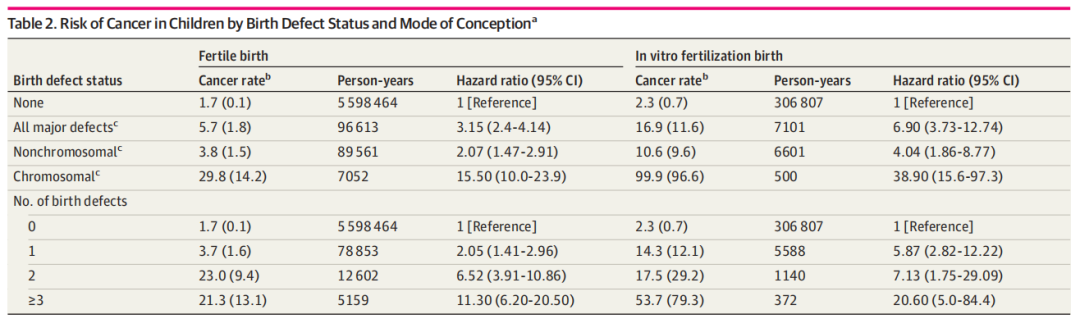
而结果也如上图所示:和正常孕育的儿童相比,通过试管婴儿技术孕育的儿童其患癌的风险更高,这个数据可以增加到200%,另外出生缺陷的发生率也会增加。
而对于这个现象的出现,研究人员也给出的一些可能的机制。
首先,可能和试管婴儿培养过程中的表观遗传学相关。在癌症的发生发展中,表观遗传学的改变都会起到很大的推动作用。当使用体外培养技术的时候,可能会导致基因表达出现变化,这将有可能导致出生缺陷和癌症发病率提高。
其次,也可能和在做体外培养的时候,细胞出现的变异有关。这时候导致癌症出现的原因就可能和细胞发生突变有关,因此对胚胎进行全基因组测序后再进行胚胎植入可以有效地避免一些儿童型癌症的出现,比如神经母细胞瘤等。
同时,在很多人的观念里面,癌症就是癌症,但是实际上成人癌症和儿童癌症有着很大的区别。
和成人肿瘤发生过程中存在很多诱因不同,儿童肿瘤的往往都和基因的改变存在联系,而也正是发病原因上的不同,儿童癌症的发生情况也会成人肿瘤大相径庭,在成年人中脑肿瘤远远低于肺癌和其他癌症,但是确实儿童最常见的肿瘤。
近些年来,伴随免疫疗法的兴起,尤其是CAR-T细胞疗法和PD-1/PD-L1抑制剂的出现,儿童肿瘤的治疗情况也得到了一定的改善。
当然这项研究也存在一定的局限性,一方面是试管婴儿严重的先天性缺陷和癌症的样本量较少,另一方面,虽然平均随访时间有5年,但是儿童肿瘤的实际发生可能需要更长时间的观察。而随着试管婴儿技术的普及,我们可能需要对技术潜在的风险进行进一步的研究,以避免一些不必要的出生风险。
原始出处:
Barbara Luke, Morton B Brown, Hazel B Nichols,et al.Assessment of Birth Defects and Cancer Risk in Children Conceived via In Vitro Fertilization in the US,JAMA Netw Open. 2020 Oct 1;3(10):e2022927. doi: 10.1001/jamanetworkopen.2020.22927.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#试管婴儿#患癌风险比自然生产增加200%!#出生缺陷#比例也更高,应该与体外过程造成一定的基因突变导致的。
46
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
52
我家就是试管婴儿,现在查出来是胶质瘤。
118
不学就无术
48
多学有益
39
#癌风险#
28
#试管婴#
41
#PE#
29
#NET#
33
#风险比#
28